While flu and RSV cases are at yearly lows in the U.S., COVID-19 infections remain high, with an estimated 550,000 daily cases. 1 of every 80 - 90 people are currently infected. If you're experiencing illness, COVID-19 is the likely culprit.
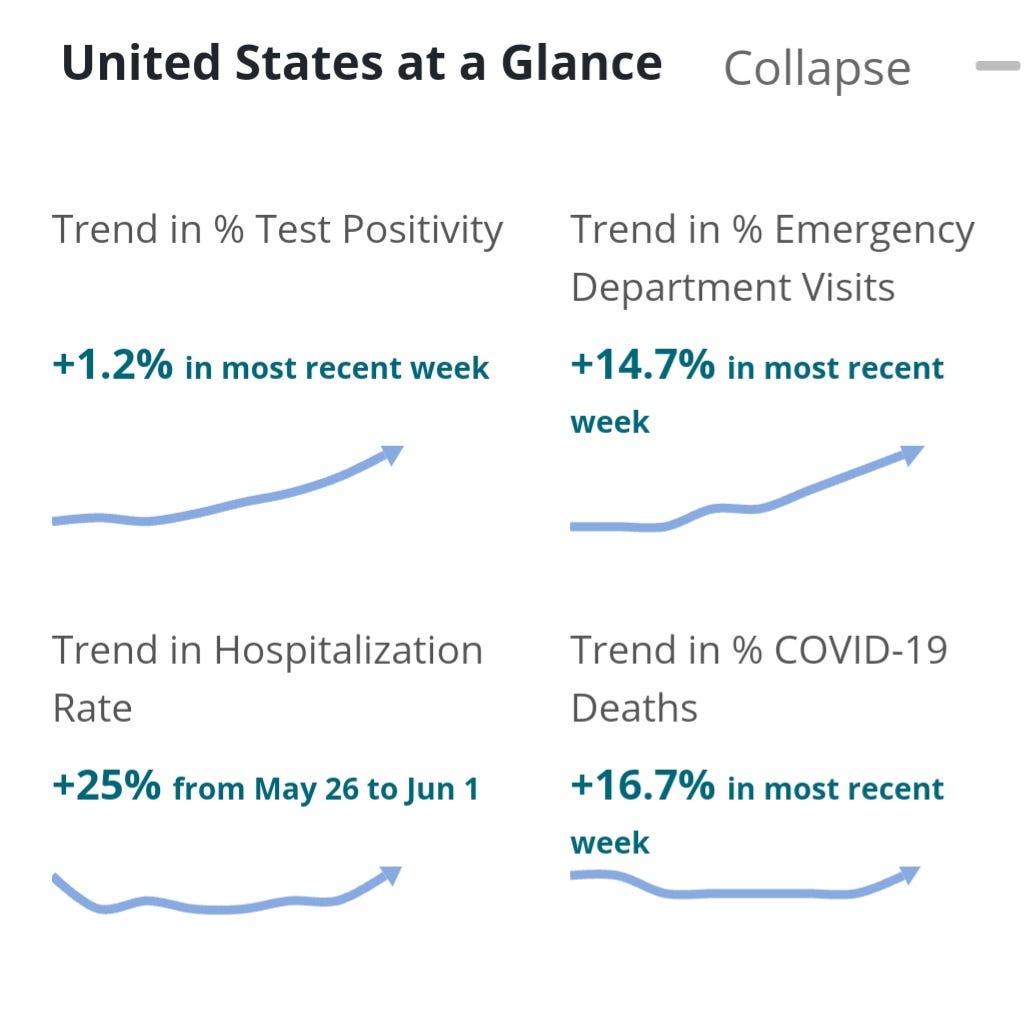
We are seeing a new surge of KP.3 sub-variants and the LB.1 variant. These variants are sending people to the hospital at an increasing rate. In the U.S., hospitalizations have increased by 25% in a week, and sadly, deaths are up by 16% over the prior week.
Common symptoms include:
Sore throat
Cough
Shortness of breath or difficulty breathing
Fatigue
Muscle or body aches
Headache
New loss of taste or smell
Congestion or runny nose
Nausea or vomiting
Diarrhea
Fever or chills
Keep in mind that on average only 15% of people were found to have fevers. A fever is an unreliable indicator for determining if it's COVID or for ending isolation. Rapid tests are the best way to know when not contagious anymore.
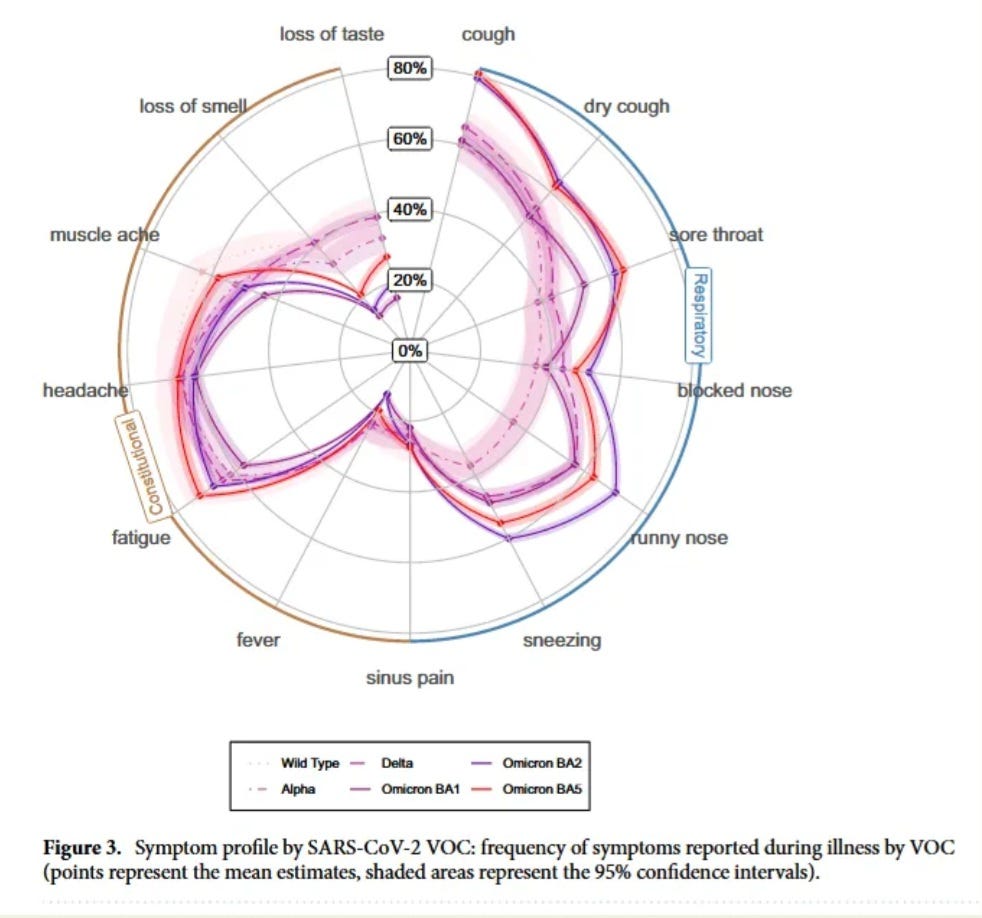
The diagram below, from a large study published in Nature, shows the percentage of people with each symptom across multiple variants. Loss of taste or smell are the only symptoms less common than a fever.
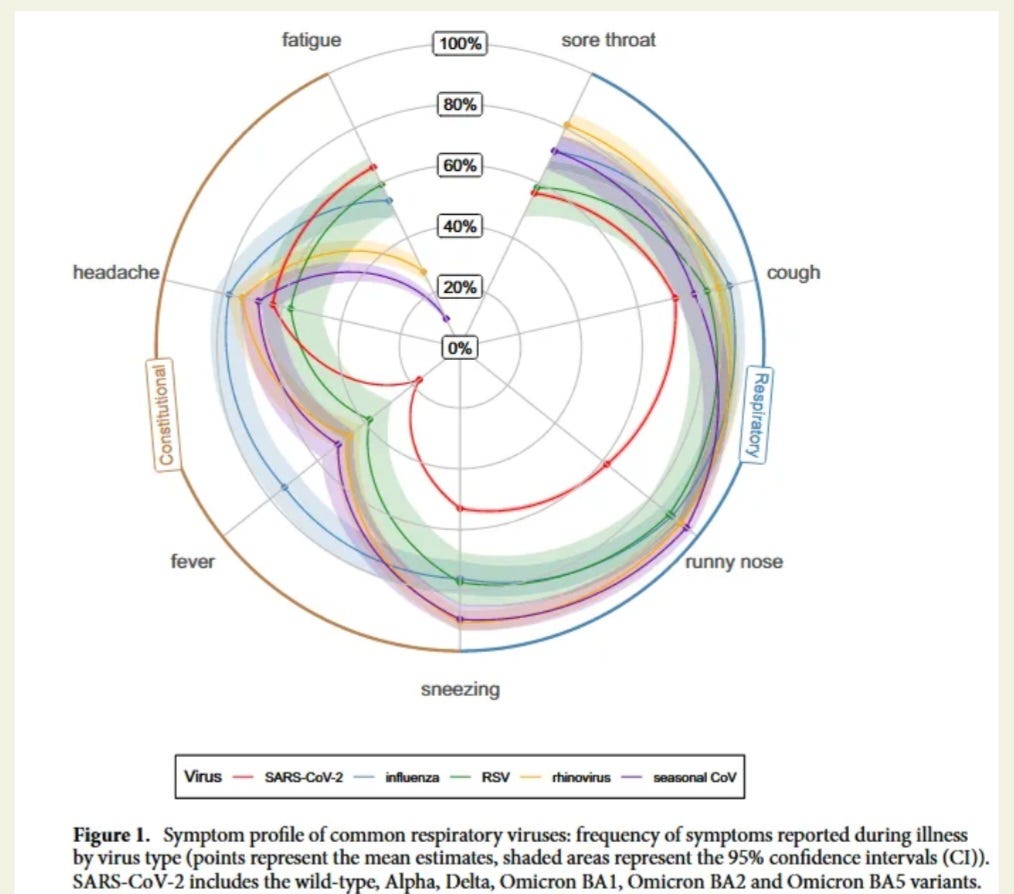
If we look below, at broader view of symptoms across multiple viruses having a fever is one of the least likely symptoms.
Symptom severity varies widely, from asymptomatic cases to those requiring hospitalization. Even asymptomatic individuals can spread the virus and potentially develop long-term health issues.
Testing remains crucial for accurate diagnosis and appropriate management of COVID-19.
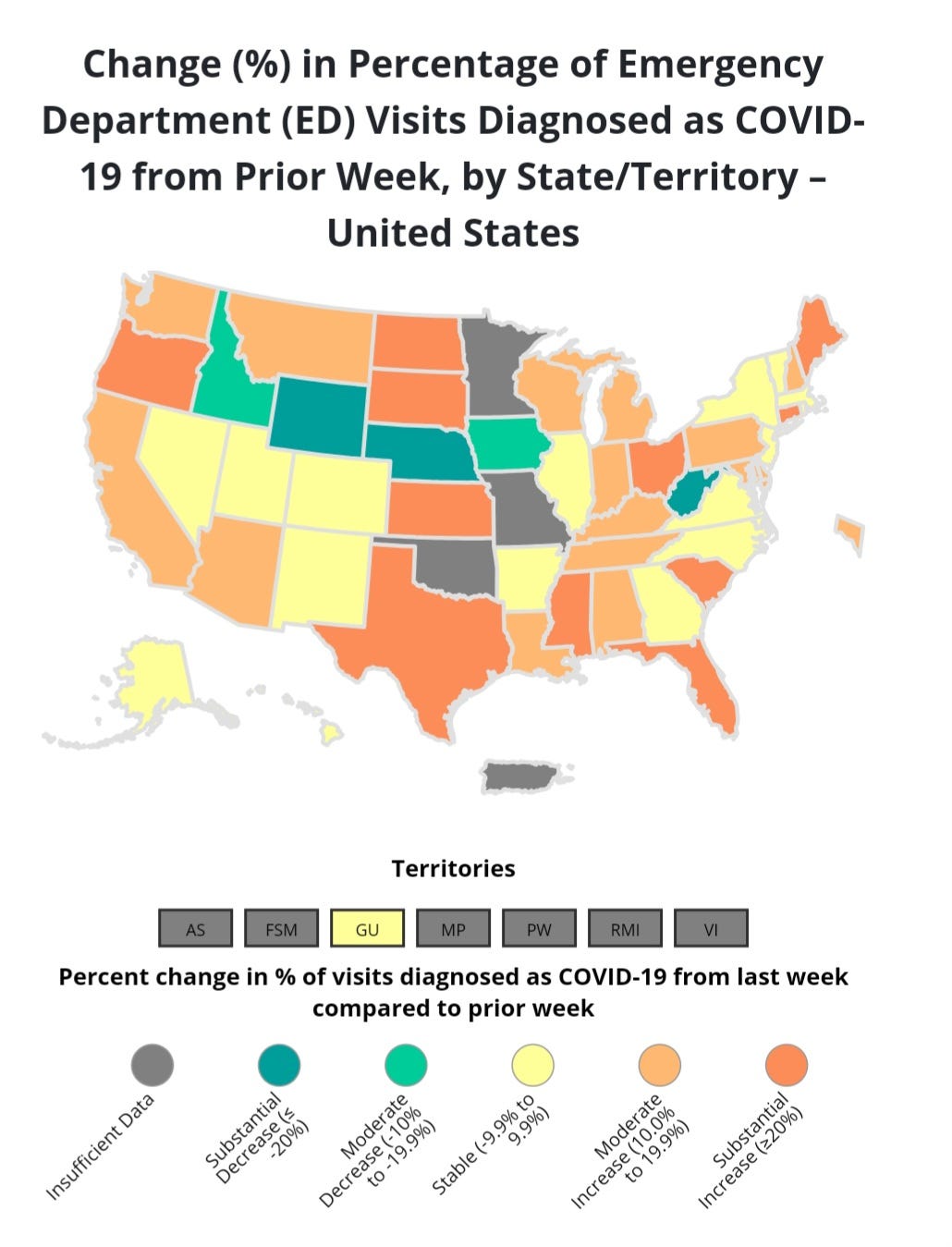
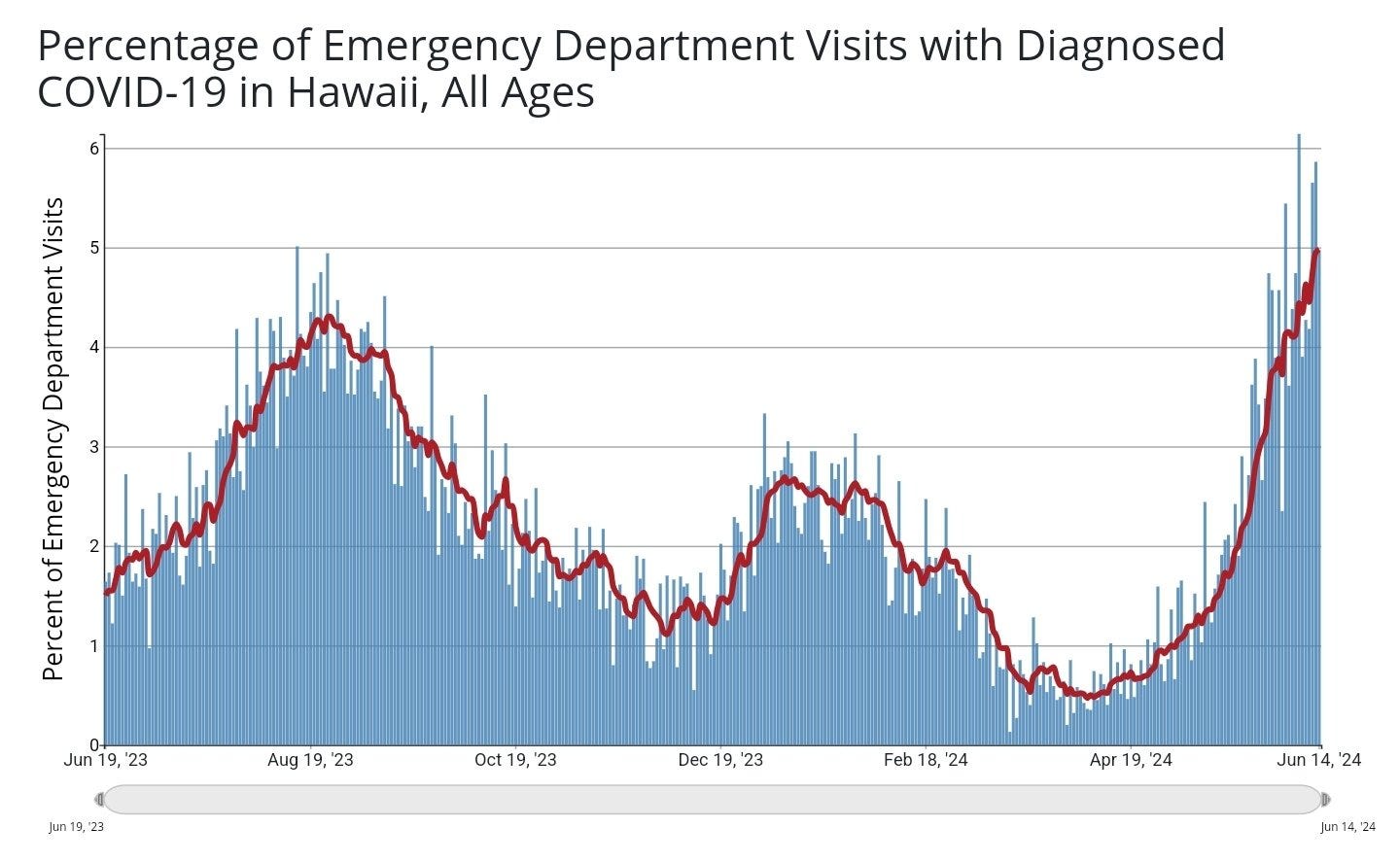
ER visits are increasing all across the U.S. These variants are more immune evasive and more likely to persist. It doesn't help that immunity from early JN.1 variants is waning in millions of people.
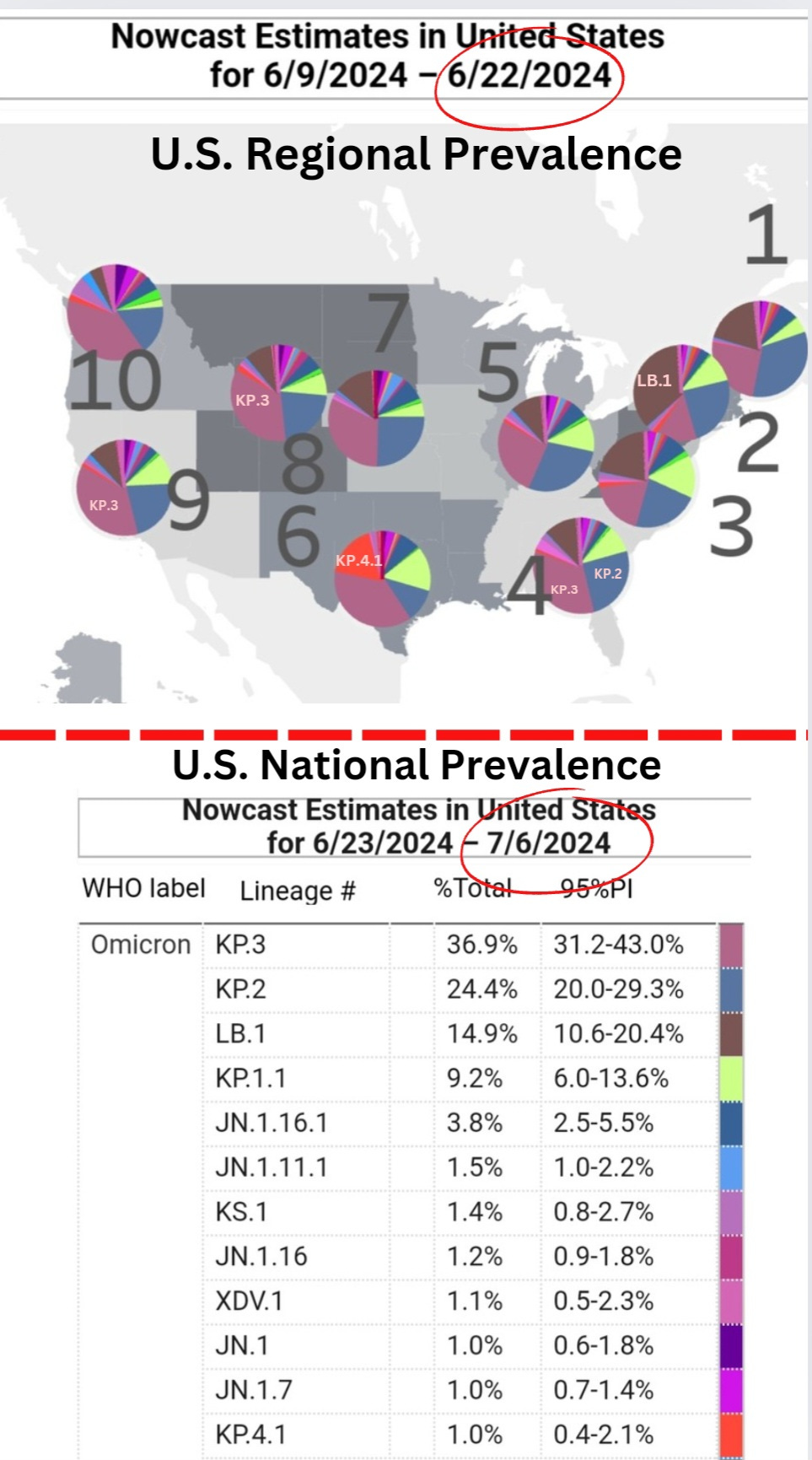
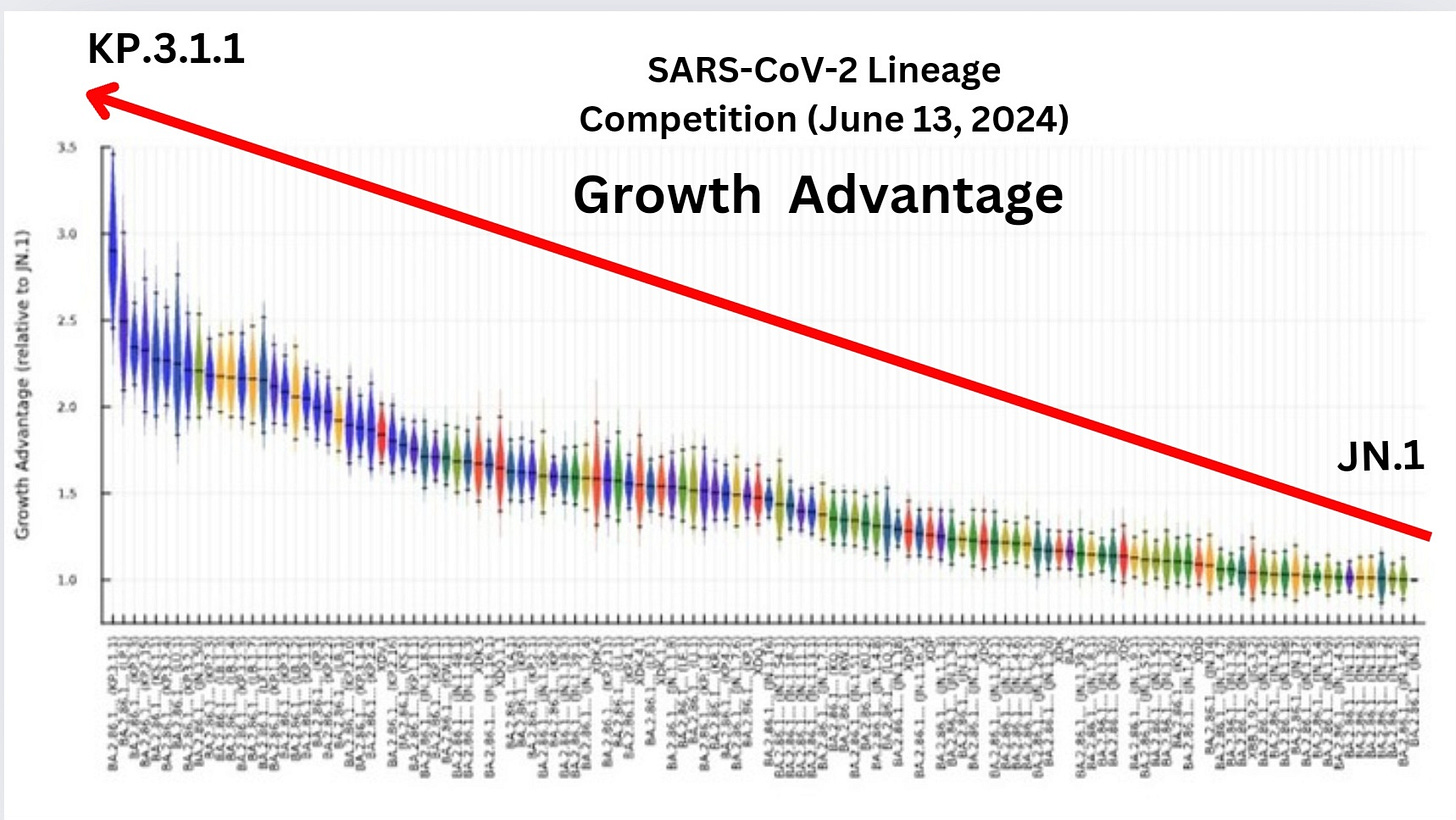
The latest CDC variant proportions shows KP.3 and it's subvariants continuing to expand in prevalence. KP.3 makes up around 37% of all cases. LB.1 is most prevalent in the Northeast. The CDC doesn't show which of the LB.1 sub-variants are in the NE. (LB.1.1 - LB.1.5) Each has unique mutations but none of them have a high enough growth advantage to out-compete the latest KP.3 sub-variants. One LB.1 sub-variant may be able to stay in the fight. LB.1.3.1 currently has a 64% growth advantage (GA), compared to the current KP.3 leader, KP.3.1.1 with a 69% GA.
KP.4.1 in region 6 is something we'll have to watch closely. While most of the KP.4.1 sub-variants can't out-compete KP.3.1.1, there is one that could potentially become dominant. KP.4.1.3 has a 75% GA but because its a newer variant that's likely to decline as more sequences come in. For example, there were only 6 sequences in the prior 10 days compared to 485 for KP.3.1.1. We'll discuss KP.3.1.1 more further down.
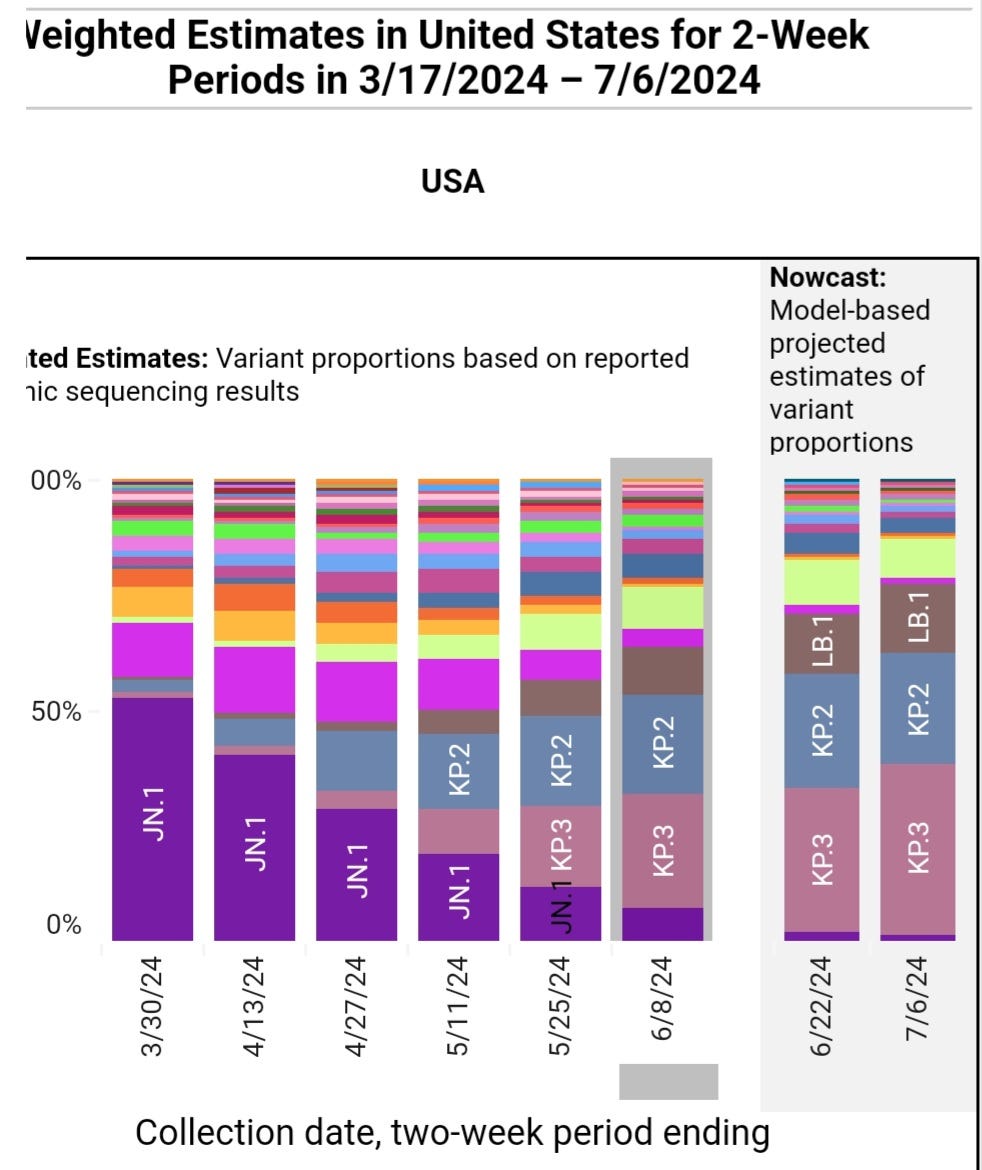
Note that JN.1 is almost completely pushed out. These variants are out-competing JN.1 which means they successfully evade the immune response people have developed to JN.1.
The KP.3 family of variants is growing, and they have mutations that allow more immune evasion and suppression of the existing immune response from vaccines and prior infections.
So far, the summer is going as expected, with the exception of the latest KP.3 sub-variants, with KP.3.1.1 surging to the highest growth advantage. This variant and some of the other KP.2, KP.3 and KP.4 sub-variants have many mutations that aren’t fully understood yet, and because of this, we should be very cautious.
In the April 21, 2024 update, TACT said, “we will see the overall prevalence going back up from mid-June through late August.”
TACT's May 6th summer forecast is what we are seeing happen now, “If you are in a country with schools that will be in session for a number of weeks, like Australia, then it is likely they will spread through schools, leading to exponential growth, and thus wastewater prevalence will increase. In the U.S., it will likely begin increasing by mid-June, possibly a little earlier, particularly in the Southern states. The prevalence will start increasing at a faster pace into July and August, and peak in the first couple weeks of September. The peak is likely to go quite a bit higher than last summer.”
Hawaii is now at the highest COVID case loads since BA.5 in summer 2022, as indicated by both the percentage of emergency department visits and wastewater prevalence. The new immune evasive and suppressive KP.3 subvariants are surging.
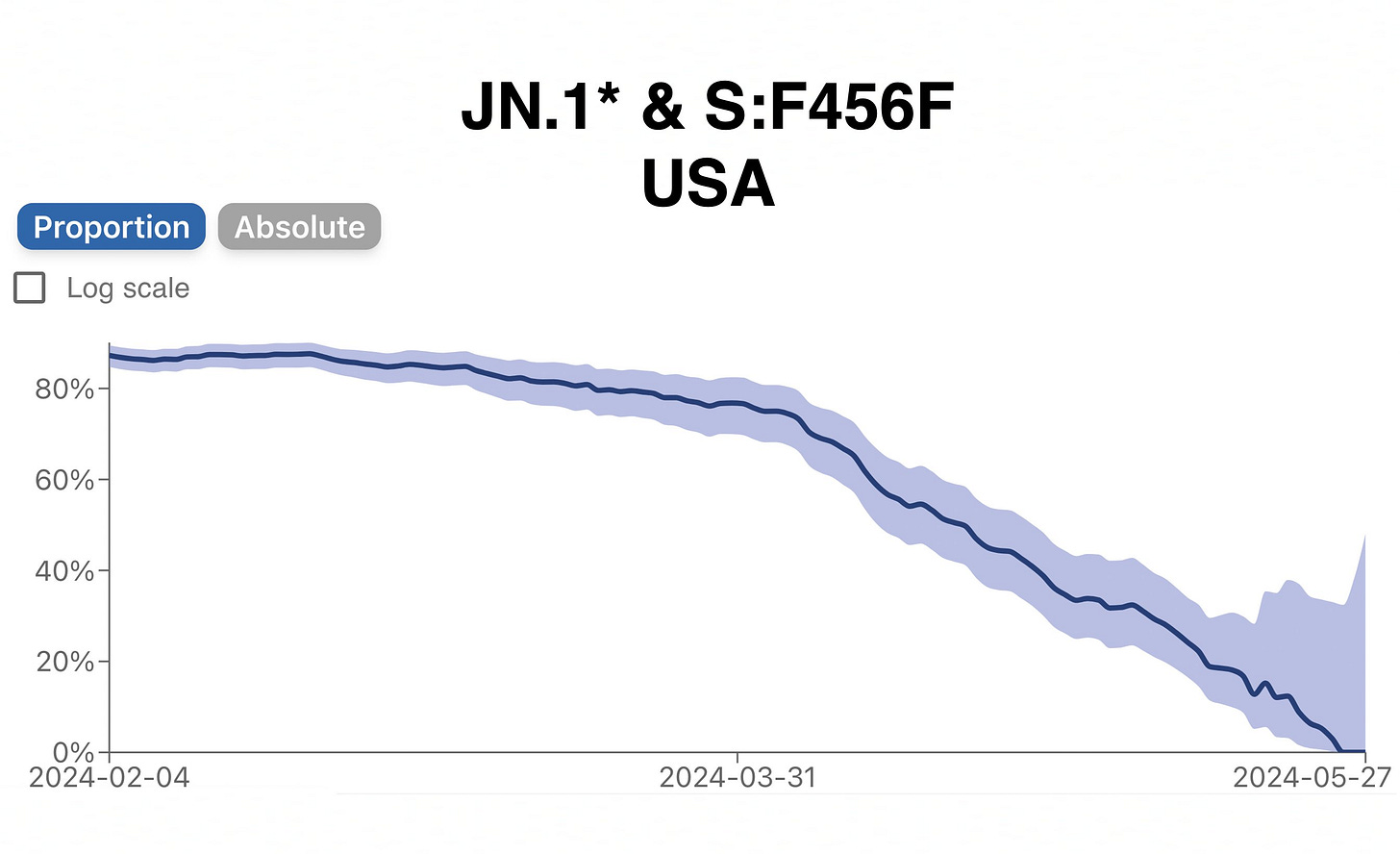
The ongoing evolution of SARS-CoV-2 continues to challenge the global immune defenses established by infections and vaccine boosters. The W.H.O.'s decision to target the JN.1 variant for the next vaccine update was a significant mistake. As we see below, JN.1 is disappearing, and as the studies show, the latest variants are already evading JN.1. The latest FDA update now recommends targeting the KP.2 variant. However, with the virus evolving so rapidly, will this update still be effective by the time it is released?
On June 10, 2024, TACT wrote, "FDA's Choice of JN.1 Variant for Upcoming COVID Vaccines in Question"
On June 13, 2024, they updated the guidance and now support the vaccines targeting KP.2. We don’t know how they decided to make this change but it is important they did. With that said, the virus is already evolving away from KP.2. The evolution is moving to rapidly for targeted vaccines to keep up. With no mitigation in place, most people have been exposed to more evolved variants than the vaccine targets, making taking a vaccine pointless, with certain exceptions for those that have managed to avoid infection. Then we have to consider that many people do not show symptoms when infected, so how do you know if you were infected? There are antibody tests, but those would only show up if infected within the prior 2 to 3 months.
Unfortunately, Novavax doesn’t have time to change its JN.1-targeted vaccine. They based the choice on the guidance of the W.H.O., but we already knew at that time, KP.2 had gained a huge advantage over JN.1
Novavax Updated JN.1 Targeted Vaccine
Novavax recently announced that their updated JN.1 vaccine induces neutralizing antibodies against multiple variants, but they did not provide supporting data. Many of these variants will likely be extinct by fall. The updated vaccines do not address changes in the N, ORF1a, ORF3a, or ORF9b proteins. For those taking extreme precautions, the vaccine might offer some protection in the fall, but its efficacy will be short-lived and likely significantly reduced. The primary benefit at this point is boosting memory T-cells after 7 to 9 months if not infected or vaccinated.
However, since most people will likely be exposed to and infected by one or more of the KP variants over the summer, an outdated vaccine may offer little benefit to most people.
Each new infection increases risks. Unfortunately, many are willingly taking this path, while others are forced due to the lack of mitigation measures to prevent children from being infected in schools. The children then infect their parents and caregivers, who in turn infect coworkers and so on. Hospitals have not adopted airborne infection prevention measures, leading to patients contracting COVID and other airborne pathogens.
On April 26, 2024, Novavax posted on its website the following:
"Our most recent nonclinical data have demonstrated that our JN.1 vaccine candidate induces neutralization responses to JN.1, JN.4, JN.1.11.1, JN.1.7, JN.1.13.1JN.1.16 strains. Our JN.1 vaccine candidate also produces polyfunctional cellular CD4+ T cell responses to a range of omicron strains, including JN.1 and JN.1.11."
Despite these claims, Novavax has not provided the necessary data to support their statements. Even if they could, the virus has already evolved beyond JN.1. The KP.2 variant can evade the immune response to JN.1 and continues to evolve, making further changes to evade the immune system.
We discussed these changes in KP.3 on May 13, 2024, when examining “The Rise of KP.3 with the S: Q493E Mutation”.
KP.3.1.1
We now face KP.3.1.1, which is short for JN.1.11.1.3.1.1. Let’s look at the growth advantage of JN.1 through KP.3.1.1 from right to left in the graph below. We can see KP.3.1.1 has taken a big leap in growth advantage and why it's able to surge, evading the immune response to JN.1 while also having a stronger ACE-2 binding ability, making infection easier.
Increasing Pace of Evolution
As more time passes, more people have persistent infections, which, in a growing number of cases, are more than one variant at the same time. Without mitigation, the virus spreads around the world faster than ever before. We can see in the radial graph above that in 2020 and 2021, when we took many precautions, the evolution was limited. In 2023, it was gaining momentum. By the end of 2023, into 2024, the evolution has exploded. As we’ll see below, the studies are already showing that KP.2 and KP.3 evade immunity to JN.1, and soon there will be variants evading immunity to KP.2, if that isn’t already happening.
Let’s take a look at the studies, the surge of KP.3 variants in various parts of the world, highlight some news stories, and discuss the White House plan that fell apart and needs reviving.
Keep reading with a 7-day free trial
Subscribe to T.A.C.T. to keep reading this post and get 7 days of free access to the full post archives.