Airborne Assault of Measles and COVID-19: A Ticking Time Bomb of Immune System Damage and Viral Evolution
COVID Variant Update: Unprecedented Immune Escape and Binding Capabilities
The convergence of measles and COVID-19 poses a significant threat, especially with evidence showing declining immunity in individuals vaccinated against measles and newborns awaiting MMR vaccination. Similar to COVID-19, heightened transmission rates increase the risk of virus evolution, potentially evading vaccines through persistent infections. Both diseases harm the immune system, with measles even erasing immunity to other pathogens. This dangerous combination of highly contagious airborne viruses demands attention.
We'll delve into these issues, including the latest COVID variants' remarkable immune escape and binding capabilities, as well as a newly emerging variant with substantial growth advantage, spreading across several countries including Canada, the U.S., the U.K., Australia, India, and Hong Kong. These latest variants likely account for the unusually high number of cases at this time, propelling COVID-19 prevalence into uncharted territory.
We'll delve into various aspects of measles and how these developments might impact us, including the impact of a new measles variant on testing efficacy, the potential for declining immunity post-measles vaccination, immune system damage caused by measles, including immune amnesia in children, and the recent CDC alert issued to U.S. clinicians regarding measles.
Additionally, we'll discuss a recent study shedding light on the extent of COVID-19 transmission among asymptomatic young adults and a study showing that Paxlovid did not reduce the risk of Long COVID. Finally, we'll provide an overview of the unfolding situation.
Unlocking vital insights through exhaustive research demands considerable time and dedication. By becoming a paid subscriber, you not only gain access to exclusive content but also play a pivotal role in sustaining this critical endeavor. Join us in our mission by becoming a valued subscriber today, ensuring that crucial information remains accessible. While our ultimate aim is to provide unrestricted access for everyone, we require additional paid subscribers to cover essential expenses. A heartfelt thank you to our existing paid subscribers for their invaluable support!
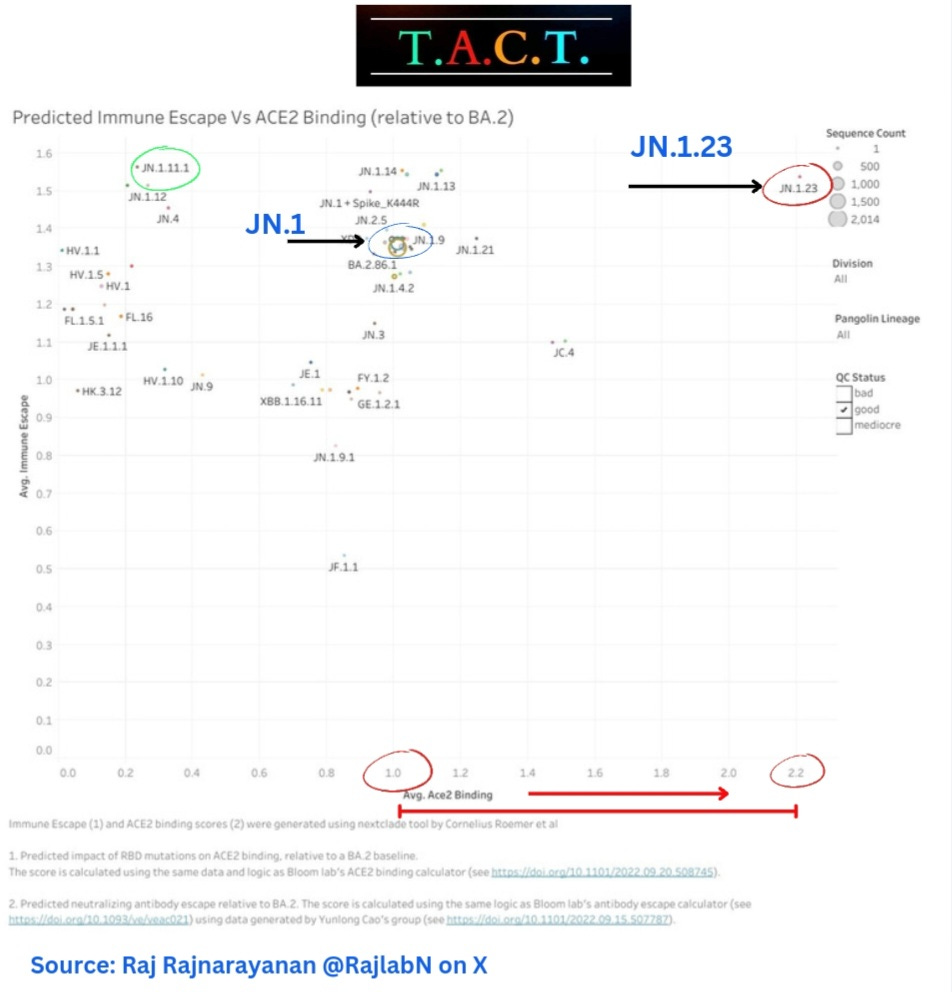
COVID Variants Update
JN.1 and its many sub-variants make up over 97% of all the variants in circulation. We are going to look at the ones gaining the most momentum. The graph below shows where each variant falls when looking at immune escape and ACE-2 binding.
The higher up on the graph, the greater the immune escape, and the further to the right, the greater the ACE-2 binding. We can see that JN.1.23 has much greater ACE-2 binding. JN.1.23 has slightly lower immune escape than JN.1.11.1 but with much greater ACE-2 receptor binding. It remains to be seen if JN.1.23 can outcompete the greater immune escape of JN.1.11.1.
JN.1.4 has an estimated growth advantage of 32% over JN.1. JN.1.11.1 has an estimated 70% growth advantage over JN.1. JN.1.23 has an estimated 67% growth advantage over JN.1.
JN.1.23’s combination of increased immune escape and ACE-2 binding may make it more dangerous than JN.1.11.1 but not necessarily more transmissible. The evolutionary track is what should be most concerning to everyone. JN.1.11.1 is already adding new mutations which may make it more dangerous than JN.1.23, but it is too early to say for sure.
KP.1 Variant (JN.1.11.1.1)
JN.1.11.1, already the fastest spreading variant, has added mutations giving it a much greater growth advantage. The new variant has been designated as KP.1 (JN.1.11.1.1) with the S:K1086R mutation. It has a growth advantage estimated to be greater than 200% over JN.1. It’s very early so this will likely decline some but the direction of evolution is continuing towards greater immune escape and a stronger binding to our cells.
How far has KP.1 spread?
There are 26 cases of KP.1 found in Canada (mostly Ontario), 2 in Queensland, Australia, 1 in Hong Kong, 1 in India, 1 in the United Kingdom, and 4 in the United States (NY, CA). We have to keep in mind that this is with limited sequencing so this variant may already be much more widespread. We can see that this very much remains a global pandemic.
CDC Variant Proportions
The latest CDC variant proportions show how extensive the JN.1 variants’ dominance is. The CDC hasn't started breaking down the many JN.1 subvariants yet.
According to the sequences from the CDC Traveler Based Surveillance Program, which includes sequencing from six airports in 5 U.S. States (California, New York, Washington, New Jersey, and Virginia), JN.1 remains the most prevalent but JN.1.4 and JN.1.11.1 are gaining ground. As shown in the chart of variants’ immune escape and ACE-2 binding above, JN.1.11.1 has the highest immune escape of any variant. We will soon find out if that remains true after we get more data on KP.1.
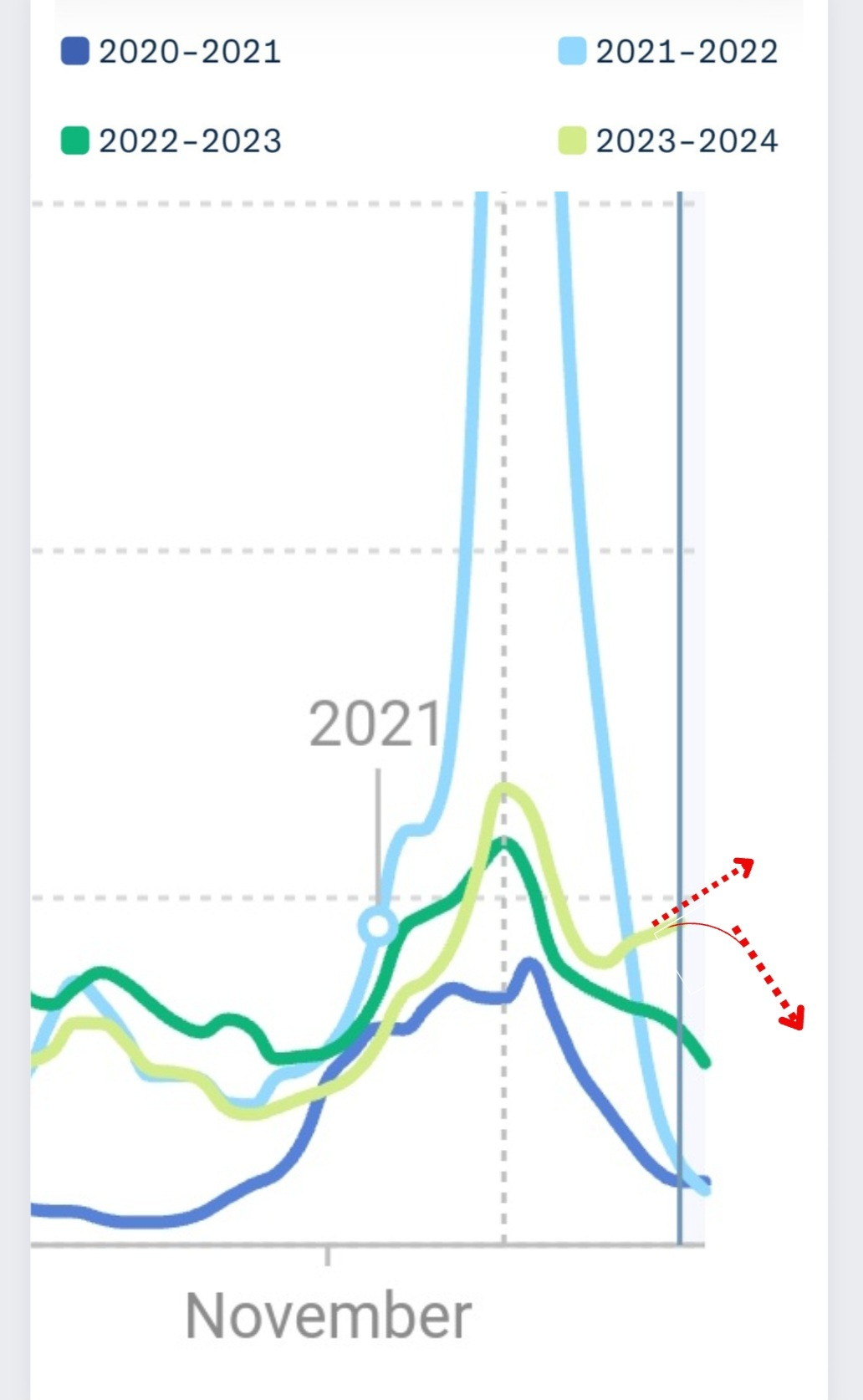
These variants may be what's behind the increasing wastewater prevalence that a majority of areas are now seeing. Remember that the overall prevalence is in uncharted territory for this time of year. Considering the increasing surge in many areas, it looks like we will remain on an increasing trajectory for a while.
Why would the CDC contemplate lifting the 5-day isolation guidance when the prevailing evidence and data indicate that most individuals remain infectious for at least 7 to 8 days?
They must revise the guidelines to stipulate a minimum isolation period of 8 days.
Paxlovid Did Not Limit Long COVID
Paxlovid did not help prevent Long COVID in the latest study. Findings on Long COVID and Symptom Rebound: (Jan 4, 2024) "Researchers found the two groups were similar. About 16% of those treated with Paxlovid had long COVID symptoms compared to 14% of those who were not treated with the medication."
“Our finding that Paxlovid treatment during acute infection is not associated with lower odds of long COVID surprised us, but it is consistent with two other rigorously conducted studies finding no difference in post-COVID conditions between 4 and 6 months after infection.” (scitechdaily.com, Feb 16, 2024)
In this study, while Paxlovid demonstrated a significant reduction in COVID-19-related hospitalizations or deaths among immunocompromised and medically at-risk patients, it failed to yield benefits for older individuals solely based on age.
Nearly 50% of Young Adults are Infectious Without Symptoms
This serves as an important reminder, corroborating findings from previous studies. Published on February 14, 2024, it underscores the inability to determine infectiousness based on symptoms alone, as a significant portion of individuals can spread the virus asymptomatically. "49.6% of individuals who had not reported a previous SARS-CoV-2 infection were seropositive to the rapid anti-SARS-CoV-2 antibody test, and 48.1% of them had neutralizing antibodies."
"These results suggest that in young adults, SARS-CoV-2 infections could be asymptomatic in a high percentage of individuals, which could contribute in part to the slow control of the current pandemic due to the large number of asymptomatic cases that are contagious and that could be a silent spread of the virus."
Do people without symptoms exhale the same or more viral particles than people with symptoms?
Yes, they can. In this study, they show that "Symptomatic and asymptomatic COVID-19 patients exhale distinctive amounts of SARS-CoV-2 not necessarily correlating with symptom severity. Particularly, asymptomatic patients might show higher exhaled breath (EB) viral shedding. Therefore, EB testing should be included in infection prevention measures as it has a high potential to reveal the most infectious individuals regardless of their symptoms during infection."
These findings emphasize the necessity of implementing tools and policies aimed at curbing airborne transmission, especially within educational and healthcare settings.
Measles Basics
Individuals most vulnerable to measles include those who are unvaccinated, unsure of their immunization status, pregnant women, and individuals with weakened immune systems due to conditions such as HIV, malnutrition, or certain medications.
Incubation time: Symptoms of measles typically manifest 7 to 14 days (avg. 10) after exposure but may appear up to 21 days later.
Symptoms: Symptoms may encompass a high fever, cough, runny nose, red and/or watery eyes, conjunctivitis, tiny white spots in the inner cheeks, gums, and roof of the mouth two to three days after symptoms begin, and a red rash, raised, blotchy usually starting on the face and spreads to the body 3 to 5 days after symptoms begin.
Potential complications of measles can involve pneumonia, brain inflammation, permanent hearing loss due to ear infections, pre-term births, and low birth weight infants.
Measles Updates
A New Measles Variant Impacting Testing
In a landscape already grappling with the relentless evolution of COVID-19 towards heightened immune evasion, the emergence of a new measles variant adds a fresh layer of complexity, with reports indicating its potential to diminish the reliability of certain measles tests.
Measles Vaccine Immunity Decline: Time for a Booster
For those between 30 and 50 years old who haven't had a recent measles booster, it's prudent to check antibody levels. A study from September 2022 suggests that vaccine-induced immunity against measles may decline over time, warranting consideration for booster shots. If antibody levels are low or non-existent, obtaining a measles booster, along with checking for antibody levels for other available boosters like varicella, is recommended.
Waning Maternal Antibodies in Newborns: Vulnerability to Measles
A 2021 study revealed that although newborns initially benefit from maternal antibodies, the gradual decline of these antibodies before measles vaccination at 9 months renders infants vulnerable to infection.
How Measles Spreads Throughout the Body
“Measles spreads rapidly from the respiratory tract to multiple organs through a cell-associated viremia fueled by extensive replication in lymphoid tissues. Virus dissemination occurs over several days during a clinically asymptomatic incubation period before the appearance of the rash. MeV replication occurs in multiple types of cells including lymphocytes, dendritic cells, macrophages, epithelial cells, and endothelial cells.”
Measles Damage to the Immune System
Measles can wipe out prior immune memory to both viruses and bacteria that people have been exposed to over a lifetime, making the situation even more dire.
A study on measles infections in children revealed that “after severe measles, children lost a median of 40% (range, 11% to 62%), and after mild measles, they lost 33% (range, 12% to 73%), of their total preexisting pathogen-specific antibody repertoires. Paired, healthy controls retained approximately 90% of their repertoires over similar or longer durations.”
Additionally, measles was found to infect 20 to 70% of memory cells, including B cells, T cells, and plasma cells in the lymphoid tissue and peripheral blood during the first 3 to 10 days after infection. If a measles infection were to precede or follow a COVID-19 infection, this damage could be significantly amplified.
Measles Persistence and Risks in Children and Immunocompromised Individuals
Like COVID-19, persistent measles infections in both children and adults can facilitate prolonged evolution, potentially evading vaccine-induced immunity. It's crucial to note that many childhood measles-related deaths stem from secondary infections rather than measles itself, as highlighted in a 2012 study. This research underscores the significance of understanding measles-induced immune suppression, which can lead to severe complications such as subacute sclerosing panencephalitis, a fatal neurological disorder caused by persistent measles virus infection. Recent studies, including one from April 2020, shed light on the mechanisms and risks associated with measles persistence, emphasizing the need for continued research and vigilance in combating this infectious disease.
It highlighted 4 main points.
“In immunocompromised patients, failure of measles virus clearance may lead to progressive lung or nervous system disease. Although infectious virus is generally cleared during the rash, this may not occur in individuals with compromised cellular immunity. For instance, individuals with congenital immunodeficiencies, HIV infection, or other types of acquired immune suppression may not develop a rash in response to MeV infection (indicating a failure of the adaptive immune response) and are at risk for developing progressive CNS infection (measles inclusion body encephalomyelitis/MIBE) and/or measles giant cell pneumonia”
“Children infected at a young age may develop subacute sclerosing panencephalitis, a progressive nervous system disease many years later.”
“Slow clearance of measles virus RNA from lymphoid tissue is associated with maturation of immune responses and lifelong immunity.”
“Slow clearance of measles virus RNA from lymphoid tissue may impair new immune responses and increase susceptibility to other infections.”
Measles: Real-World Impacts Unfold
A 30-fold Increase of Measles in the European Region
In a December 14, 2023 report from the W.H.O., they say, “The WHO European Region is experiencing an alarming rise in measles cases. Over 30,000 measles cases were reported by 40 of the Region’s 53 Member States between January and October 2023. Compared to 941 cases reported in all of 2022, this represents a more than 30-fold rise. The rise in cases has accelerated in recent months, and this trend is expected to continue if urgent measures are not taken across the Region to prevent further spread.
“We have seen in the Region not only a 30-fold increase in measles cases but also nearly 21,000 hospitalizations and 5 measles-related deaths. This is concerning” explained Dr Hans Henri P. Kluge, WHO Regional Director for Europe. “It is vital that all countries are prepared to rapidly detect and timely respond to measles outbreaks, which could endanger progress towards measles elimination.”
Measles Outbreaks: Disproportionally Impact Children - 4 Out of Every 5 Cases
In 2023, measles has impacted individuals across all age groups, with notable variations in the age distribution of cases among different countries. On the whole, 2 out of 5 cases were observed among children aged 1 to 4 years, while another 2 out of 5 cases were reported among individuals aged 5 to 19 years. Adults aged 20 years and older accounted for 1 out of every 5 cases. During the period from the beginning of the year to October, there were 20,918 hospitalized cases reported, with two countries documenting five measles-related deaths.
Measles Clinician Alert from the CDC
On Jan 25, 2024, the CDC issued an alert to clinicians regarding measles outbreaks, yet the approach to "control" airborne transmission in schools remains unaddressed. They alert doctors who may or may not read it. This is especially concerning in light of a new variant capable of evading testing, underscoring the necessity for public awareness. If measles is evolving enough to diminish test sensitivity, could it also be evading immunity with greater ease? We don’t know these answers yet, so we should be proactively taking every step possible to reduce transmission.
The alert says, "Between December 1, 2023, and January 23, 2024, the Centers for Disease Control and Prevention (CDC) was notified of 23 confirmed U.S. cases of measles, including seven direct importations of measles by international travelers and two outbreaks with more than five cases each. Most of these cases were among children and adolescents who had not received a measles-containing vaccine (MMR or MMRV), even if age eligible.”
Note: The CDC states that “most” were among unvaccinated children. How many were vaccinated? Hopefully, they make this distinction clearer in updates.
"Due to the recent cases, healthcare providers should be on alert for patients who have: (1) febrile rash illness and symptoms consistent with measles (e.g., cough, coryza, or conjunctivitis), and (2) have recently traveled abroad, especially to countries with ongoing measles outbreaks. Infected people are contagious from 4 days before the rash starts through 4 days afterward."
School Impacts and Closures
The recent closure of ten primary schools in the health zone of Rety, Ituri, due to the resurgence of bubonic plague and measles, underscores the severity of the situation. More than three thousand children are affected, prompting school and health authorities to intensify response measures to safeguard the community. While this scenario currently unfolds in the Democratic Republic of the Congo, the looming question remains: how long until similar crises emerge elsewhere in the world?
Measles Reported in 15 U.S. States in 2024
NBC News reports on February 24, 2023, “Measles is a 'heat-seeking missile' experts warn as Florida outbreak grows” “A seventh case, the first in a child under age 5, follows the state’s controversial surgeon general’s decision to let parents decide whether to quarantine children or keep them in school.”
The Centers for Disease Control and Prevention reported that as of Friday there have been at least 35 measles cases in 15 states in 2024 — most related to international travel. In January, there were nine measles cases in Pennsylvania, eight of them in Philadelphia. (If there are no more cases reported there as of early next week, the Philadelphia outbreak will be declared over.) Late Friday, Michigan’s health department announced that it, too, had identified a measles case — its first since 2019.
T.A.C.T.’s Overview:
Public health agencies worldwide have failed to address the risk of airborne transmission and viral evolution, as evidenced by recent developments in Florida. Dr. Joseph Ladapo, Florida's Surgeon General, allowed parents to decide whether to quarantine their children amid rising measles cases. Unlike COVID-19, which has a shorter incubation period, measles can remain latent for up to 14 days, increasing the risk of outbreaks. If the testing might be missing more cases due to a new measles variant, the number of infections may be much higher.
Indiana and Michigan reported their first cases of measles in 5 years, in just the past two days. The recent case of an Indiana resident seeking care for measles at three Chicago hospitals highlights the urgent need for effective airborne infection prevention measures in healthcare settings. Without such measures, the risk of transmission remains high, particularly among immunocompromised patients who inadvertently become hosts for persistent infections, potentially leading to further mutations and viral evolution.
The co-circulation of COVID-19 and measles poses a significant threat, potentially compromising immune systems and facilitating viral persistence and mutation. The emergence of immune-evasive JN.1 sub-variants exacerbates this risk, increasing the likelihood of Long COVID and immune system weakening. Concerningly, increasing flu cases signal a lack of attention to airborne transmission prevention measures, and potentially more people with weakened immune systems, resulting in preventable hospitalizations and deaths.
According to the Feb. 23, 2024 update from the CDC Flu report, seasonal influenza activity remains elevated nationally, with unexpected increases observed in certain regions. Additionally, the report highlights nine more child deaths attributed to flu-related illnesses, underscoring the preventable nature of these fatalities.
Every infection increases risks and shortens our lives, so any immunity gained comes at a great cost. Measles and COVID-19 act as ticking time bombs, eroding immune defenses, persisting in more individuals, and driving viral evolution if left unchecked. Prioritizing ventilation, air filtration, and evidence-based guidance is essential to mitigating risks and preventing severe outcomes. Proactive measures, such as wearing N95/P100 masks and using air purifiers, coupled with advocacy for comprehensive public health interventions, are crucial in addressing the heightened risk from airborne viruses.
Share your thoughts, questions, stories, insights, and/or information.






TACT...Nice photograph at the top. If that photograph doesn't scream 'FRESH AIR' , I don't know what does.
I enjoyed your quixotic hope in reference to the Center for Disease Circulation ("How many were vaccinated? Hopefully, they make this distinction clearer in updates.")
Don't hold your breath, TACT.
Regarding the JN.1 quasispecies swarm, see the last line in this reference.
There is something different about the JN.1 swarm, perhaps in the enzymes it is using to potentiate infection that have not yet been completely elucidated.
https://www.biorxiv.org/content/10.1101/2024.02.14.579654v1
Lastly, while you mentioned measles (which is definitely a problem), don't sleep on DENGUE.
To the folks in Florida and Texas, all I can say is "SUMMER IS COMING"
Thanks for your tireless work.
Fascinating. If not, slightly depressing update, but forewarned is forearmed. I’m particularly interested in the study on Paxlovid. As a lay person I’m making my way through it and having trouble understanding if they adequately accounted for all confounding variables. I see it mentioned BMI is a significant piece of missing data. age might be another. I thought I saw a vague reference to including that in the demographics, but wasn’t 100% clear. On a surface level, it seems hard to understand that a drug that dramatically and quickly reduces viral load in your body couldn’t be at least somewhat helpful for long-term downstream effects. The study didn’t look at what we now know are some of the most common long Covid symptoms as well, such as cognitive impairment/brain, fog, exercise, intolerance and PEM. Would love for people more experienced than I am in reading through study methodology to comment on how solid the conclusions of the study might be.