The CDC's Updated Guidance: A Departure from Science-Based Logic
The CDC's Declining Relevance and Struggle for Effectiveness
One key distinction between COVID-19 and diseases like measles or influenza lies in their response to antibodies. While antibodies from vaccines or prior infections effectively target and neutralize measles, flu, and many other pathogens, COVID-19 can evade neutralizing antibodies within a few months, if not faster. This evasion enables COVID-19 to replicate, spread, and establish itself within viral reservoirs before the immune system's T-cells can eradicate infected cells.
Persistent infections provide the virus with opportunities to adapt to treatments and immune responses from vaccines. When a new variant infects someone with a persistent infection, it can undergo further adaptations through recombination, exchange, and mutation before spreading to others. The more individuals experience persistent infections, the higher the likelihood of these recombinant events occurring, accelerating the pace of viral evolution.
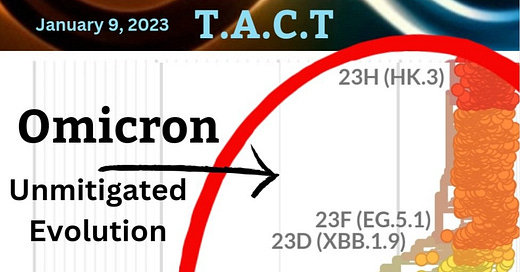
The included image, dated January 2023, serves as a stark reminder of the consequences of reducing mitigation measures, illustrating the trajectory we've reached due to such actions.
The pace of COVID-19's evolution surpasses the rate at which treatments and vaccines can keep up, posing significant challenges. Their recent efforts to align COVID guidelines with those for other respiratory infections, as stated by CDC Director Mandy Cohen, aim for simplicity and clarity in recommendations. However, this approach raises concerns when considering diseases like measles.
Both measles and COVID-19 are highly contagious airborne viruses, with airborne particles remaining in the air of an unventilated space for 2 to 3 hours after the infected person left the room.
Both measles and COVID-19 can infect nearly every cell type of the immune system, and weaken it. They both infect lymphocytes (T-cells and B-cells), dendritic cells, macrophages, epithelial cells, endothelial cells, and neurons.
We have effective vaccines for measles, but not for COVID-19.
COVID immunity wanes to infection within 2 to 3 months. T-cell response limits severity for up to 10 months but starts waning after 6 months. On the other hand, measles immunity to infection wanes remains strong for 20 to 40 years.
COVID leads to Long COVID, for which we don't have any treatments.
Measles is spreading, which is concerning, yet largely contained. COVID is completely out of control and infecting millions every week, hospitalizing tens of thousands and killing thousands every week.
By what logic does it make sense to reduce the isolation guidance for COVID-19 but not measles? The Washington Post reported, “Many businesses already stopped offering workers with COVID infections five paid days to isolate and celebrated state officials who moved away from the CDC guidance, arguing it was overly burdensome to keep workers with mild or no symptoms off the job for so long.” The CDC seems to prioritize economic interests over public health.
Even voices within public health, like David Margolius, Cleveland's health official, endorse the CDC's updated guidance, advocating for uniform treatment of respiratory viruses. However, this blanket approach fails to account for the distinct characteristics and impacts of each virus, raising doubts about its efficacy. Neglecting the nuanced differences among infectious diseases risks undermining public health efforts and eroding trust in decision-making processes.
"Simplifying the public health messaging to treat all of these dangerous contagious respiratory viruses the same makes a lot of sense." - David Margolius
The CDC's failure to prioritize evidence-based approaches undermines its effectiveness and relevance in safeguarding public health. Accountability is essential, as public health decisions should serve the interests of all citizens, not just select stakeholders.
The CDC is making itself ineffective and irrelevant. We cannot let this stand because public health is falling off a cliff. They must be held accountable.
It’s more important than ever to understand the risk of repeated COVID-19 infections and how those infections happen.
This article is a comprehensive resource, compiling numerous recent studies spanning the past two years, emphasizing the importance of understanding its content for safeguarding our children's future. Delving into the health impacts and transmission dynamics of COVID-19 in children, but also pertains to adults.
In part I, we address the risks posed to children by COVID-19 and the implications of repeated infections. In part II, we examine the transmission patterns of SARS-CoV-2, underscoring its spread within schools and homes among both symptomatic and asymptomatic individuals.
Safeguarding Children: COVID's Impact on Children's Health and Understanding Airborne Transmission
Understanding the risk of repeated COVID-19 infections and how those infections happen is of critical importance. This article compiles numerous recent studies spanning the past two years, emphasizing the importance of understanding its content for safeguarding our children's future. Delving into the health impacts and transmission dynamics of COVID-19 in children, we are using a question-and-answer framework.
Does SARS-CoV-2, the virus that causes COVID-19, spread by respiratory droplets in exhaled breath (EB) that become airborne, potentially lingering in the air for hours?
Yes, numerous studies have underscored the ability of each infectious individual, regardless of symptoms, to exhale millions of viral particles per hour.
A study published in 2020 highlights this, stating, "Our study demonstrates that exhaled breath emission plays an important role in SARS-CoV-2 emission into the air, which could have contributed greatly to the observed airborne cluster infections and the ongoing pandemic. Accordingly, measures such as enhanced ventilation and the use of face masks are essential to minimize the risk of infection by airborne SARS-CoV-2."
Since then, extensive data has further confirmed the significant exhalation of viral particles by infected individuals within a short timeframe. As noted in a recent study by Northwestern Medicine, "COVID patients exhale high numbers of virus during the first eight days after symptoms start, as high as 1,000 copies per minute"
This study provides the first longitudinal, direct measure of the number of SARS-CoV-2 viral copies exhaled per minute throughout the infection, demonstrating the substantial viral load emitted.
Furthermore, the study reveals that "On day eight, exhaled levels of virus drop steeply, down to near the limit of detection — an average of two copies exhaled per minute." Interestingly, it's observed that while mildly and moderately symptomatic patients with COVID exhale large amounts of virus, severely symptomatic cases exhale higher levels on average. Additionally, vaccinated and unvaccinated patients exhibit similar levels of viral exhalation over the infection course.
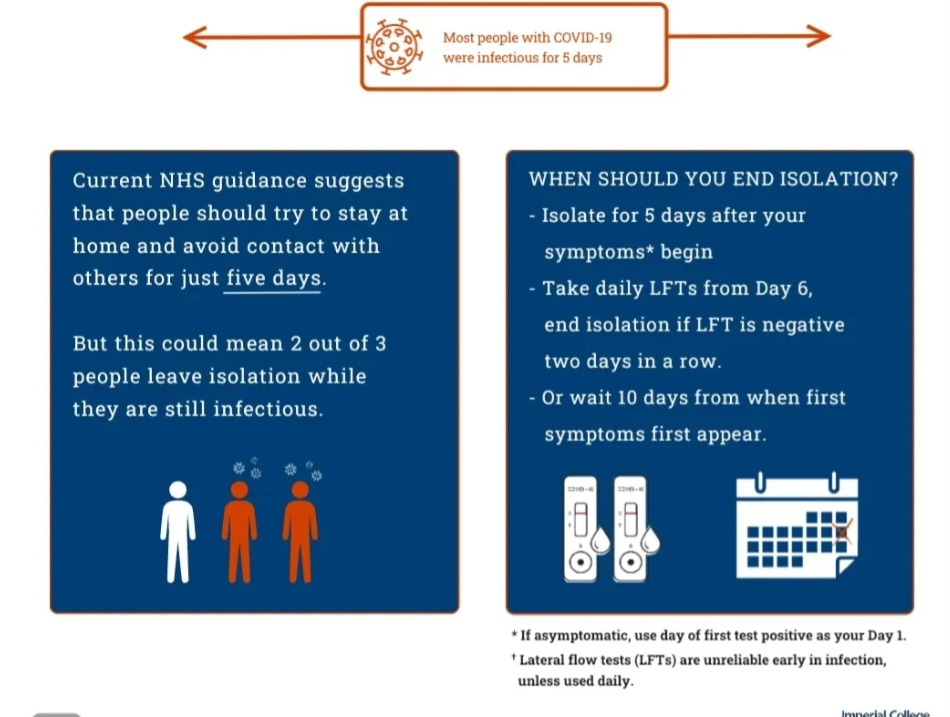
A real-world study led by the Imperial College London and published in The Lancet Respiratory Medicine journal found that in people who develop symptoms, the majority are not infectious before symptoms appear, but two-thirds of cases remain infectious five days after symptom onset. This was during earlier variants, but again confirming most people were still infectious on day 5.
These findings, along with numerous other studies, consistently indicate that individuals typically remain infectious for a minimum of 7 to 8 days, with a considerable number remaining infectious for 10 to 20 days.
A significantly more effective approach, rooted in scientific evidence, is outlined in the graphic above from the Imperial College of London. It suggests a protocol of isolating for 5 days followed by testing on day 6 to assess continued infectiousness. Repeat testing on day 7 helps confirm the results. If negative, it's likely that the individual is no longer infectious and can safely end isolation. However, if the test is positive, continued isolation is necessary.
Following isolation, it's recommended to use a quality N-95 or similar mask for an additional 2 to 3 days while interacting with family members or being in public spaces to further reduce the risk of transmission.
It's particularly crucial to highlight this approach in light of the recent CDC update on isolation guidance. The shift from the previously recommended 5-day isolation period to just 24 hours after a fever, without testing, lacks scientific basis and isn’t grounded in logic. It should be retracted immediately. Failure to do so could have detrimental effects on all levels of society.
Share your thoughts, questions, stories, insights, and/or information.






Thank you for this summary. When people ask me if they should get vaccinated for the first time, or get the booster from 2023, or vaccinate their children, I have no answer. Is a vaccine targeting an extinct variant better than nothing? I don’t know. Public health, of course, says to get vaccinated. Our vaccines are years behind the virus. Americans die every day from covid, and we don’t hear about their preventable deaths. Because as a society, we have decided not to prevent preventable deaths, whether from guns, drugs, domestic violence or viruses…
Pathetic is what it is