Safeguarding Children: COVID's Impact on Children's Health and Understanding Airborne Transmission
Many people underestimate the connection between COVID-19 and other airborne pathogens and the long-term health issues they can cause in children. What's often overlooked is just how frequently children encounter these viruses and bacteria in school settings. Let's explore this further by addressing some commonly misunderstood questions.
Before delving into those questions, let's take a moment to reflect on the survival rate of children before people advocated for improved public health measures. Up until the past 100 years or so, nearly half of all children didn't survive to adulthood. However, in the last century, there has been remarkable progress. Global newborn survival rates have soared from 50% to 96%, largely due to efforts to prevent infectious diseases. Looking at historical data, in France between 1600 and 1700, approximately, 40% to 50% of children died. In Sweden between 1750 and 1780, nearly 40% of children didn't survive past the age of 15. Similarly, paleodemographers analyzing skeletons in modern-day Peru estimate that almost half of children born two millennia ago perished before puberty. It's striking to consider that until relatively recently, such high childhood mortality rates were commonplace, a fact we often overlook today.
What were the changes that increased the odds of survival? It started with the landmark Public Health Act of 1848, enacted in the U.K., marking a significant milestone in efforts to reduce child mortality. This legislation, championed by Edwin Chadwick, laid the foundation for state responsibility in managing public health by prioritizing clean water, proper sanitation, and effective waste management.
Chadwick used economic rationale to emphasize the long-term cost-effectiveness of improving people’s health. Improving health would reduce the need for government relief typically provided to families affected by infectious diseases. This is a lesson that applies today. Key measures advocated included enhanced drainage, sewer provision, refuse removal, and the appointment of medical officers in towns. Cholera outbreaks, and sustained advocacy led to the passage of the Public Health Act of 1848.
People have had to advocate for quality public health ever since. It has never been willingly provided by the people in power. Without advocacy, we may have gone another 1,000 years with half of all children dying. This is why advocacy work is so important.
Airborne Transmission of Many Respiratory Viruses
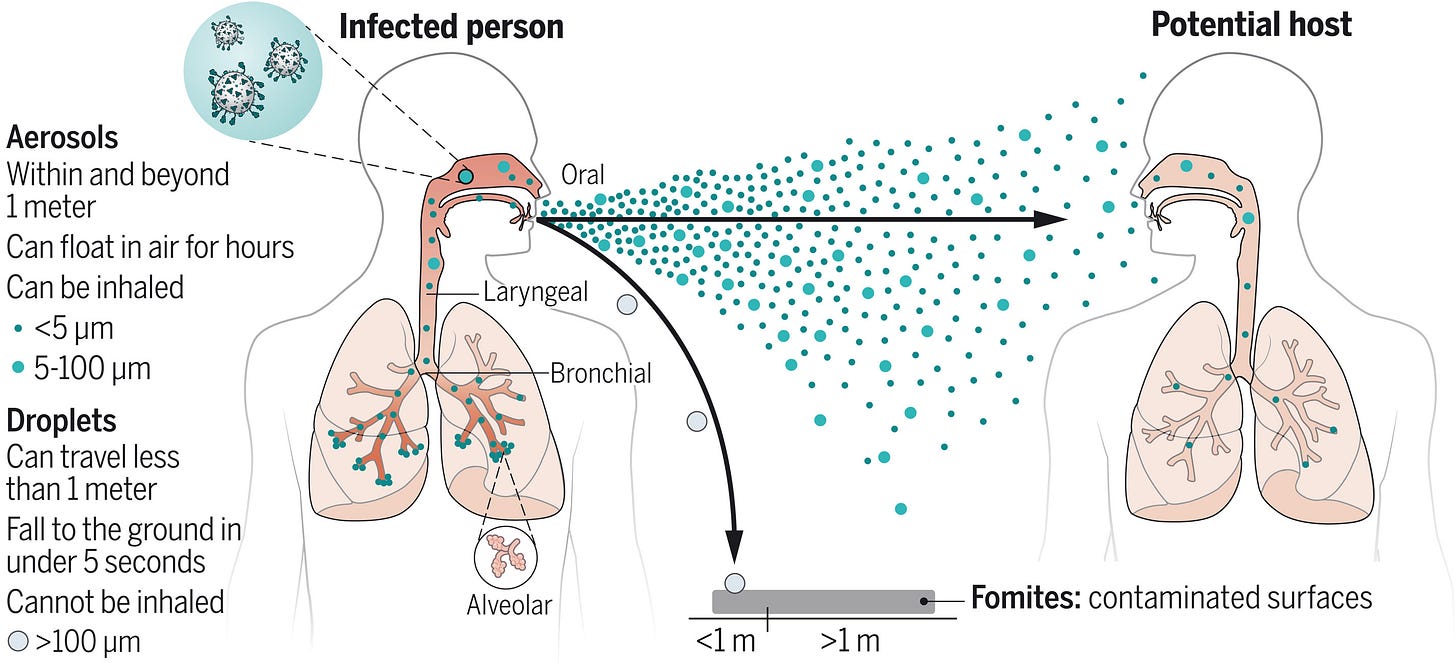
Most people don’t know that all of these respiratory viruses are spread via aerosolized respiratory droplets, that can remain airborne for extended periods. The significance of airborne transmission in spreading pathogens has been vastly underestimated, largely due to inadequate understanding of aerosol behavior and, in part, to the misinterpretation of anecdotal evidence. Studies have provided compelling evidence supporting the airborne transmission of various respiratory viruses, including measles virus, influenza virus, respiratory syncytial virus (RSV), human rhinovirus (hRV), adenovirus, enterovirus, severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome coronavirus (MERS-CoV), and SARS-CoV-2.
"These results suggest that contrary to current opinion, rhinovirus transmission, at least in adults, occurs chiefly by the aerosol route." (The Journal of Infectious Diseases, September 1987)
Airborne transmission has been estimated to contribute to approximately half of influenza A virus transmission in household settings, underscoring the significant role of airborne transmission in the spread of respiratory pathogens.
Given our understanding of how we had to advocate for better public health measures and the confirmed airborne transmission of not only COVID-19 but also numerous other viruses and bacteria, prioritizing measures that ensure clean air for kids in schools and hospitals emerges as the most pivotal investment in our collective future. By doing so, we have the potential to prevent a myriad of chronic illnesses, enhance educational outcomes, elevate the quality of life in later years, and ultimately extend life expectancy. As we will see below, failing to take action yields precisely the opposite outcome.
Understanding the risk of repeated COVID-19 infections and how those infections happen is of critical importance.
Below, we will go over numerous recent studies from the past two years, emphasizing the importance of understanding its content for safeguarding our children's future. We will look at the many health impacts and the transmission dynamics of COVID-19 in children. We are using a question-and-answer framework, that will hopefully be more helpful.
In part I, we address the risks posed to children by COVID-19 and the implications of repeated infections. In part II, we examine the transmission patterns of SARS-CoV-2, underscoring its spread within schools and homes among both symptomatic and asymptomatic individuals.
Unlocking vital insights through exhaustive research demands considerable time and dedication. By becoming a paid subscriber, you play a pivotal role in sustaining this critical endeavor. Join us in our mission by becoming a valued subscriber today, ensuring that crucial information remains accessible. A heartfelt thank you to our existing paid subscribers for their invaluable support!
"The toll of chronic illness on children often remains hidden from public view, but its impact is profound, affecting every aspect of their lives."
"Behind the smiles of children with chronic illness lies a daily struggle, battling pain and uncertainty while striving for normalcy."
I. COVID-19’s Impact on Children's Health
1. Can COVID-19 harm children's immune systems, opening the door to other infections?
Yes, COVID-19 can indeed impair the immune systems of both children and adults. A study published in October 2023 examined 228,940 children aged 0-5 years who had no prior respiratory syncytial virus (RSV) infection. The findings were also confirmed in a separate study involving 370,919 children of the same age group, with no prior RSV infection, who had medical encounters from July 2021 to August 2021, during a non-overlapping period.
Researchers concluded that COVID-19 was linked to a significantly higher risk of RSV infections among children aged 0-5 years in 2022. Similar results were observed in the study population of children aged 0-5 years in 2021. These findings suggest that COVID-19 may have contributed to the surge in RSV cases in young children in 2022 due to a large accumulation of COVID-19-infected children and the potential long-term adverse effects of COVID-19 on the immune and respiratory systems.
2. How does COVID-19 make children more susceptible to other infections?
We know that COVID-19 has been listed as one of the leading causes of Lymphocytopenia. "People with lymphocytopenia experience recurrent infections or develop infections with unusual organisms & it is a risk factor for the development of cancers & autoimmune disorders." Lymphocytopenia refers to a condition where you have a lower-than-normal level of lymphocytes in your blood. Lymphocytes are a type of white blood cell that plays a crucial role in your immune system. They help your body fight off infections by:
Identifying and destroying foreign invaders, such as viruses and bacteria.
Helping to produce antibodies, which are proteins that target and neutralize specific pathogens.
Regulating the immune response and preventing it from attacking healthy tissues.
Therefore, a low lymphocyte count can weaken your immune system and make you more susceptible to infections. Causes of lymphocytopenia can vary and include viral infections such as HIV/AIDS, COVID-19, and Epstein-Barr virus (EBV). Other causes include some bacterial infections, malnutrition, certain medications, and bone marrow problems like aplastic anemia and leukemia. (see below: COVID can infect bone marrow)
Lymphocytes come in different subtypes classified by their appearance, function, and developmental pathway:
T lymphocytes (T cells): These make up about 70-80% of total circulating lymphocytes. They mature in the thymus gland and play a central role in cell-mediated immunity, directly attacking infected cells, cancer cells, and foreign invaders. T cells are further subdivided into several types: helper T cells (Th cells), cytotoxic T cells (Tc cells), regulatory T cells (Tregs), and memory T cells.
B lymphocytes (B cells): These makeup about 15-20% of total circulating lymphocytes. They mature in the bone marrow and specialize in humoral immunity, producing antibodies that specifically target and neutralize pathogens and toxins in the bloodstream and tissues.
Natural killer (NK) cells: These make up about 5% of total circulating lymphocytes. Although technically not true lymphocytes (they don't develop in the thymus), NK cells share some morphological and functional similarities with lymphocytes. They lack specific immune receptors but play a crucial role in innate immunity by directly killing infected cells, cancer cells, and certain pathogens without prior sensitization.
3. Could lymphocytopenia be overlooked if not requesting the right test?
Yes. Symptoms of lymphocytopenia can be vague and non-specific. Frequent infections, fatigue, fever, and night sweats are all common symptoms that can arise from various other conditions. Therefore, unless these symptoms are severe or persistent, a doctor might not immediately think to order a CBC with differential.
Lymphocytopenia is diagnosed through a complete blood count (CBC) test. Lymphocytopenia may be overlooked if the doctor orders a standard CBC test (CBC without differential) because lymphocytes account for only 20 to 40% of the total white blood cell count. Without a differential means that the total count of white blood cells is reported without specifying detailed information about white blood cell subtypes like lymphocytes, neutrophils, eosinophils, basophils, and monocytes. The standard CBC test (CBC without differential) is less expensive but it doesn’t offer the level of detail that a CBC test with differential does.
If you are concerned about lymphocytopenia, you can discuss it with your doctor and request a complete blood count (CBC) with differential.
According to the MSD manual, in adults, the normal lymphocyte count ranges from 1000 to 4800/mcL (1 to 4.8 × 109/L, while in children under 2 years, the normal count is 3000 to 9500/mcL (3 to 9.5 × 109/L). By the age of 6, the lower limit of normal is 1500/mcL (1.5 × 109/L). It's worth noting that normal values may vary slightly between different laboratories.
The majority of blood T cells, around 65%, are CD4+ (helper) T cells. Therefore, individuals with lymphocytopenia often exhibit reduced absolute numbers of T cells, particularly CD4+ T cells. In adult blood, the average count of CD4+ T cells is approximately 1100/mcL (with a range of 300 to 1300/mcL [1.1 × 109/L with a range of 0.3 to 1.3 × 109/L]), while the average count of the other major T-cell subgroup, CD8+ (suppressor) T cells, is around 600/mcL (with a range of 100 to 900/mcL).
4. Is there evidence showing that COVID-19 can infect the thymus and bone marrow, where T-cells and B-cells mature?
COVID-19 not only depletes these important cells but can potentially infect the thymus where T-cells mature and bone marrow where the B-cells mature.
“SARS-CoV-2 can directly target the thymus and alter gene expression profile of thymic epithelium."
5. Is there evidence showing that COVID-19 can persist in children’s tonsils and adenoids even if they didn’t have any symptoms during the acute phase of the infection?
Yes. Tonsils and adenoids are major sites of persistent COVID infections in children without any symptoms. The tonsils and adenoids are important for the development of the immune system. We don’t know how many kids this is impacting or how many more it will impact. This study also suggests that persistent infections in the tonsils may play an important role in community transmission. “Lymphoid tissue can be a reservoir of SARS-CoV-2 and may play an important role in community dissemination.”
6. Is there evidence showing that COVID-19 could lead to long-term immune system damage in children?
A study published in January 2023, looked at mild and asymptomatic cases of COVID-19 in children and adult family members and how this impacted the immune systems of children. All consented samples used in these analyses were collected between July 23 and October 24, 2020, so before the vaccines were used for anyone looking to blame vaccines.
They found that "adults but not children develop robust memory T cell responses to SARS-CoV-2." Children do not have the same memory T-cell protection that adults develop, so that would leave them more exposed to reinfections, or it means they are using more naïve T-cells and damaging the development of the naïve T-cells that accumulate until puberty.
This study found that patients who had COVID-19 were 42.63% more likely to develop autoimmunity.
COVID-19 impacts everyone’s immune system to varying degrees. Some people recover faster than others, but it can take weeks to more than eight months to recover.
For young children, the consequences could be more profound. COVID-19 may be causing irreversible damage to children’s immune systems.COVID-19 could disrupt the crucial development of naïve T-cells, potentially reducing the quality and duration of their lives.
"SARS-CoV-2 can directly target the thymus and alter gene expression profile of thymic epithelium."
7. Can COVID-19 damage children's lungs?
Yes, COVID-19 can lead to widespread functional lung alterations in children and adolescents. "Low-field-strength MRI showed persistent pulmonary dysfunction in children and adolescents who recovered from COVID-19 and those with long COVID."
Babies are being born with smaller lungs, increasing the risk of viruses like RSV and flu, with an array of potential issues in the future.
8. Can COVID-19 damage children's liver?
Yes, we have studies on COVID-induced liver injury in infants, children, and adolescents.
"The spectrum of liver injury in children with COVID-19 ranges from being asymptomatic with elevated serum transaminase levels to severe liver injury, with reports of acute-on-chronic liver failure in patients with underlying liver disease." (published June 9, 2023)
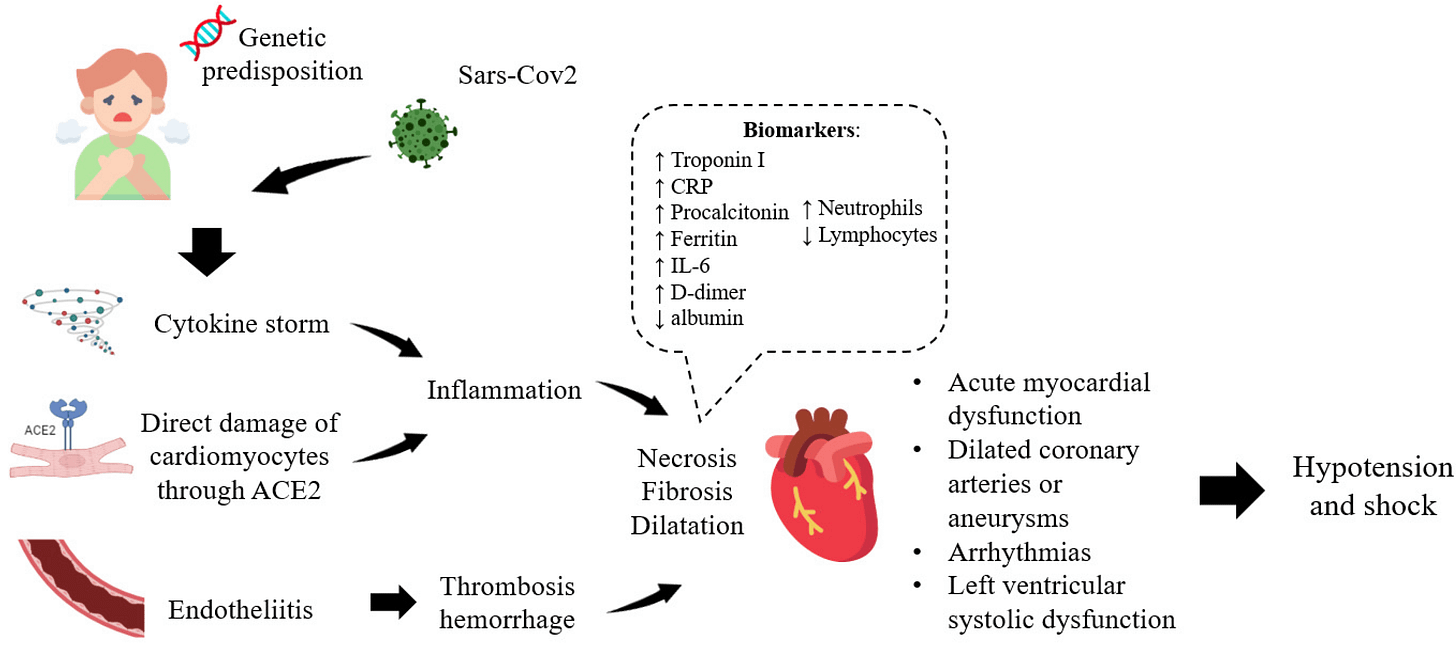
9. Can COVID-19 cause heart damage in children?
Yes. COVID is causing heart dysfunction in previously healthy children. Many children are dealing with heart damage, such as heart lesions and mid and long-term atrioventricular functional changes.
10. Is there evidence of COVID-19 causing small blood clots and vascular dysfunction, that can also impact the brain and kidneys?
Yes. Thrombotic Microangiopathy (TMA) is a serious medical condition characterized by a specific pattern of damage that can occur in the smallest blood vessels within vital organs, most commonly affecting the kidneys and brain. TMA involves thrombosis (formation of blood clots) in capillaries and arterioles due to endothelial injury (damage to the lining of blood vessels).
“Defects in the blood vessel wall lining can produce rough patches that are like potholes on a road – they can slow traffic and cause a lot of damage. Red blood cells can become deformed and then burst. Platelets can activate and cause clots to form. The wreckage from all these events can close off entire blood vessels. In the end, parts of your kidney can die from lack of blood flow, and your body can run low on red blood cells and platelets.”
In the normal kidney, there are small blood vessels called capillaries lined with endothelial cells.
When these endothelial cells become damaged, blood flow through the kidney slows down.
The effects include:
Deformed red blood cells that may burst.
Activation of platelets leading to clot formation.
Closure of entire blood vessels, causing parts of the kidney to die due to insufficient blood flow
A study titled, “Evidence of thrombotic microangiopathy in children with SARS-CoV-2 across the spectrum of clinical presentations” was published on December 8, 2020, in Blood Advances. This study included 50 children admitted to the Children's Hospital of Philadelphia (CHOP) with confirmed SARS-CoV-2 infection between April and July 2020.
Key findings:
Elevated levels of a biomarker called soluble thrombomodulin (sTM) were found in all participants, regardless of disease severity. sTM is associated with a condition called thrombotic microangiopathy (TMA), which involves blood vessel damage and clotting.
These findings suggest that SARS-CoV-2 infection may contribute to cardiovascular complications in children, even in those with mild disease.
sC5b9 plasma levels are elevated in children with SARS-CoV-2 infection, even if they have minimal symptoms of COVID-19.
A high proportion of children with SARS-CoV-2 infection met clinical criteria for TMA.
They found that the children showed signs of terminal complement activation with various levels of SARS-CoV-2 infection. Terminal complement activation is the last step in a series of immune responses, where complement proteins form a membrane attack complex on target cells, causing cell lysis and destruction. While crucial for fighting pathogens, excessive activation can lead to tissue damage and inflammation, contributing to autoimmune disorders and infections. Increases in a substance called sC5b9, which is linked to this process, happened regardless of other COVID-19 markers. This increase was also linked to signs of kidney problems. Testing for sC5b9 may be another way to show an ongoing infection is occurring.
Source: A study in "Pediatrics" on cardiovascular complications in children with MIS-C: https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.120.049836
11. Is there evidence showing that COVID-19 can damage the kidneys?
Yes. COVID-19 can damage the kidneys in several ways.
"Kidney damage is a serious and life-threatening complication that could arise from severe COVID-19"
"The kidneys play a crucial role in filtering and balancing the blood, maintaining homeostasis, and regulating many important functions in the body"
"Treatment for COVID kidney may include medications or even dialysis"
Symptoms of kidney damage from COVID:
-Reduced urine production, although sometimes urine production remains unchanged
-Accumulation of fluid leading to swelling in the legs, ankles, or feet
-Breathlessness
-Tiredness
-Mental confusion
-Nausea and vomiting
-Lack of strength
-Irregular pulse
-Chest discomfort or tightness
-Seizures or loss of consciousness in severe instances.
What causes kidney damage with COVID?
Kidney cell targeting: COVID-19 may infect the cells of the kidneys, as the cells have receptors that allow the virus to attach and invade, potentially causing damage to the tissue. This is similar to what has been observed in the lungs and heart.
Oxygen deprivation: In severe COVID-19 cases, patients may experience abnormally low levels of oxygen in the blood, which can lead to kidney malfunction. This is often due to pneumonia.
Cytokine storms: The body's extreme immune response to the virus can lead to a cytokine storm (cytokine is a cell signaling substance), where a sudden influx of cytokines causes severe inflammation. While trying to fight the infection, this reaction can also destroy healthy tissue, including that of the kidneys.
Blood clotting: COVID-19 can cause small clots to form in the bloodstream, which can clog the smallest blood vessels in the kidneys and impair their ability to filter toxins, excess water, and waste products from the body.
If kidney failure is suspected, you'll likely need to be hospitalized. You may undergo the following treatments depending on how COVID affects your kidneys:
Medications play a crucial role in managing acute kidney failure. IV fluids may be administered if fluid levels in the blood are low, while diuretics can help eliminate excess fluid in cases of swelling. To regulate potassium levels, medications such as calcium, glucose, or sodium polystyrene sulfonate may be prescribed to prevent dangerous elevations. In cases of low calcium levels, calcium infusions may be recommended. Dialysis may be necessary to remove toxins and excess fluid, as well as to regulate potassium levels, through a process where blood is filtered outside the body and purified before being returned.
Source: https://ada.com/covid/covid-19-symptom-kidney-pain/
Another source of information:
National Kidney Foundation.
Kidney disease & COVID-19
https://www.kidney.org/coronavirus/kidney-disease-covid-19#miracle-cures-and-treatments
12. Does COVID-19 increase the risk of diabetes in children?
Yes. The CDC published a report in January 2022 that stated, “Persons aged <18 years with COVID-19 were more likely to receive a new diabetes diagnosis >30 days after infection than were those without COVID-19 and those with prepandemic acute respiratory infections. Non–SARS-CoV-2 respiratory infection was not associated with an increased risk for diabetes.”
The CDC also stated, “The increased diabetes risk among persons aged <18 years following COVID-19 highlights the importance of COVID-19 prevention strategies in this age group”
13. Can COVID-19 infect bone marrow, leading to a change in bone structure?
Yes. "In vitro and preclinical studies suggest that SARS-CoV-2 may directly infect bone marrow cells, leading to alterations in bone structure and osteoclast numbers."
"SARS-CoV-2 and its Multifaceted Impact on Bone Health: Mechanisms and Clinical Evidence" (Published: 18 January 2024)
How will this impact the growing bones of children and will it damage the immune system considering that the bone marrow is where B-cells are processed and memory B-cells are stored for longer duration immune responses? We don’t know these answers but we can’t ignore these potential risks.
14. Do COVID-19 infections have a direct impact on children's mental health?
Yes. COVID-19 impacts children's mental health in many ways.
COVID's impact extends to mental health, with the developing minds of children at risk of both short-term and long-term issues. A study published in Nature, titled, "Para-infectious brain injury in COVID-19 persists at follow-up despite attenuated cytokine and autoantibody responses", found that "Neurological complications of COVID-19 are associated with evidence of neuroglial injury in both acute and late disease and these correlate with dysregulated innate and adaptive immune responses acutely"
Examining the neurological effects of SARS-CoV-2 infections in children, a study released on February 14, 2023, sheds light on concerning findings. It reveals, “COVID-19 in the pediatric population is mostly asymptomatic. However, 1 out of 5 children presents non-specific neurologic symptoms such as headache, weakness, or myalgia. Furthermore, rarer forms of neurological diseases are increasingly being described in association with a SARS-CoV-2 infection. Encephalitis, stroke, cranial nerve impairment, Guillain-Barré syndrome, or acute transverse myelitis have been reported and account for around 1% of pediatric COVID-19 cases. Some of these pathologies may occur during or after the SARS-CoV-2 infection.”
While some might downplay the severity by noting that “only” 1% of children are more severely affected, this overlooks the significant impact. With approximately 72.5 million children in the U.S. alone, “only” 1% translates to 725,000 children facing potentially serious neurological issues. In a typical school district of 10,000 students, this means 100 may suffer from such problems. Given the risks to developing brains and the evolving nature of SARS-CoV-2, it's unacceptable to ignore these consequences.
15. Is there evidence showing that COVID-19 can impact the brain and memory?
Yes. A study published on June 29, 2023, explores the long-term effects of SARS-CoV-2 on the brain and memory. It reveals that “during the past 3 years, an estimated 10–15% of SARS-CoV-2 patients had shown the post-COVID-19 symptoms (namely, Long-COVID syndrome), including fatigue, hyposmia, shortness of breath, headache, smell or taste disturbance, myalgia, anxiety, and brain fog (memory impairment and other cognitive symptoms).”
Of particular concern is the finding that “SARS-CoV-2 can invade the neural system to interfere with human memory.” This raises alarms from both an educational and human perspective.
The cumulative impact on children’s memory, brain development, and overall health from repeated infections during critical developmental years is alarming. Considering the potential for multiple infections over time, this could lead to a generation of young adults facing a myriad of health and mental health challenges. The repercussions are far-reaching and demand attention and action.
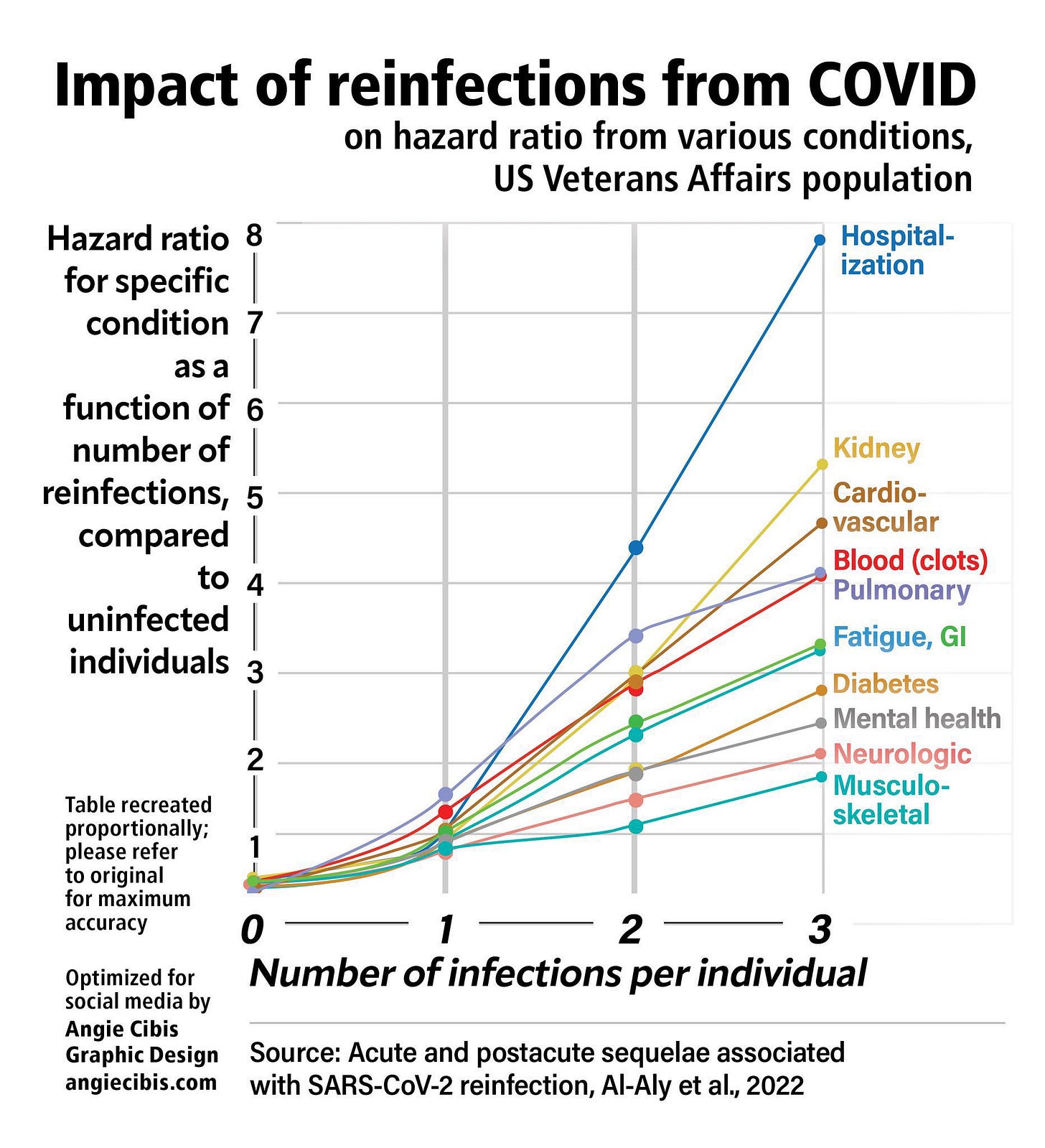
16. Does every infection with COVID-19 increase risks to long-term health?
Yes, the risks increase with the number of infections.
The data presented in the graph stems from an extensive study involving over 5 million individuals, primarily sourced from the VA database. However, it's crucial to note that this risk extends beyond adults to children, who can act as carriers and bring the virus home to vulnerable family members.
Even with conservative estimates suggesting that 10% of children may experience long-term health complications, this translates to 500 children in a school district with 5,000 students. To illustrate, consider a family with two elementary school-aged children, aged 6 and 8, amid the current infection rates. Such a family could potentially endure at least 10 or more symptomatic infections before their children graduate. Each infection episode not only results in missed school days but also escalates the risk of adverse outcomes for all household members.
It's imperative to recognize the broader ramifications of this situation. Transmission doesn't confine itself within the school walls. Beyond the long-term health implications, missing a week or two of school disrupts education, while the corresponding absence from work jeopardizes both the health and financial stability of families.
17. Can COVID-19 cause pink eye-like symptoms, including conjunctivitis?
Yes. A study from 2021, found the presence of SARS-Cov-2 in tears and conjunctiva of patients with COVID-19. They conclude that ocular transmission is possible and preventative measures should be taken.
Children, in particular, may be more susceptible to eye infections of COVID due to their proximity to others and their tendency to touch surfaces and then rub their eyes.
Read more details on how COVID-19 evades the eye’s immune defenses here.
18. Can COVID-19 persist for weeks or months in children that had no symptoms or mild symptoms and can it lead to Long COVID in kids?
Yes. For some families, the cost of a COVID-19 infection can last for months or years.
"Our analysis suggests that in children, independent from disease severity, SARS-CoV-2 can spread systemically and persist for weeks to months. Viral RNA has been documented in children who have died from critical acute disease, but also in pediatric patients diagnosed with multisystem inflammatory syndrome weeks to months after previous asymptomatic or mild infection with SARS-CoV-2." (published in the Lancet, June 26, 2023)
"Today, Long COVID in the pediatric population is a significant and real problem. Without a doubt, all children with suspected or documented COVID-19 infection and their parents, even in the absence of symptoms at the time of diagnosis, should be informed about the possible persistence of symptoms for more than 4 weeks and their possible reappearance after the acute phase. It should be remembered that girls and adolescents with comorbidities, including psychiatric conditions, are associated with a higher risk of prolonged COVID-19."(published January 6, 2023)
(also see LongCOVIDKids.org)
II. Airborne Transmission of SARS-CoV-2 and Other Pathogens
1. Does SARS-CoV-2, the virus that causes COVID-19, spread by respiratory droplets in exhaled breath (EB) that become airborne, potentially lingering in the air for hours?
Yes, numerous studies have underscored the ability of each infectious individual, regardless of symptoms, to exhale millions of viral particles per hour.
A study published in 2020 highlights this, stating, "Our study demonstrates that exhaled breath emission plays an important role in SARS-CoV-2 emission into the air, which could have contributed greatly to the observed airborne cluster infections and the ongoing pandemic. Accordingly, measures such as enhanced ventilation and the use of face masks are essential to minimize the risk of infection by airborne SARS-CoV-2."
Since then, extensive data has further confirmed the significant exhalation of viral particles by infected individuals within a short timeframe. As noted in a recent study by Northwestern Medicine, "COVID patients exhale high numbers of virus during the first eight days after symptoms start, as high as 1,000 copies per minute"
This study provides the first longitudinal, direct measure of the number of SARS-CoV-2 viral copies exhaled per minute throughout the infection, demonstrating the substantial viral load emitted.
Furthermore, the study reveals that "On day eight, exhaled levels of virus drop steeply, down to near the limit of detection — an average of two copies exhaled per minute." Interestingly, it's observed that while mildly and moderately symptomatic patients with COVID exhale large amounts of virus, severely symptomatic cases exhale higher levels on average. Additionally, vaccinated and unvaccinated patients exhibit similar levels of viral exhalation over the infection course.
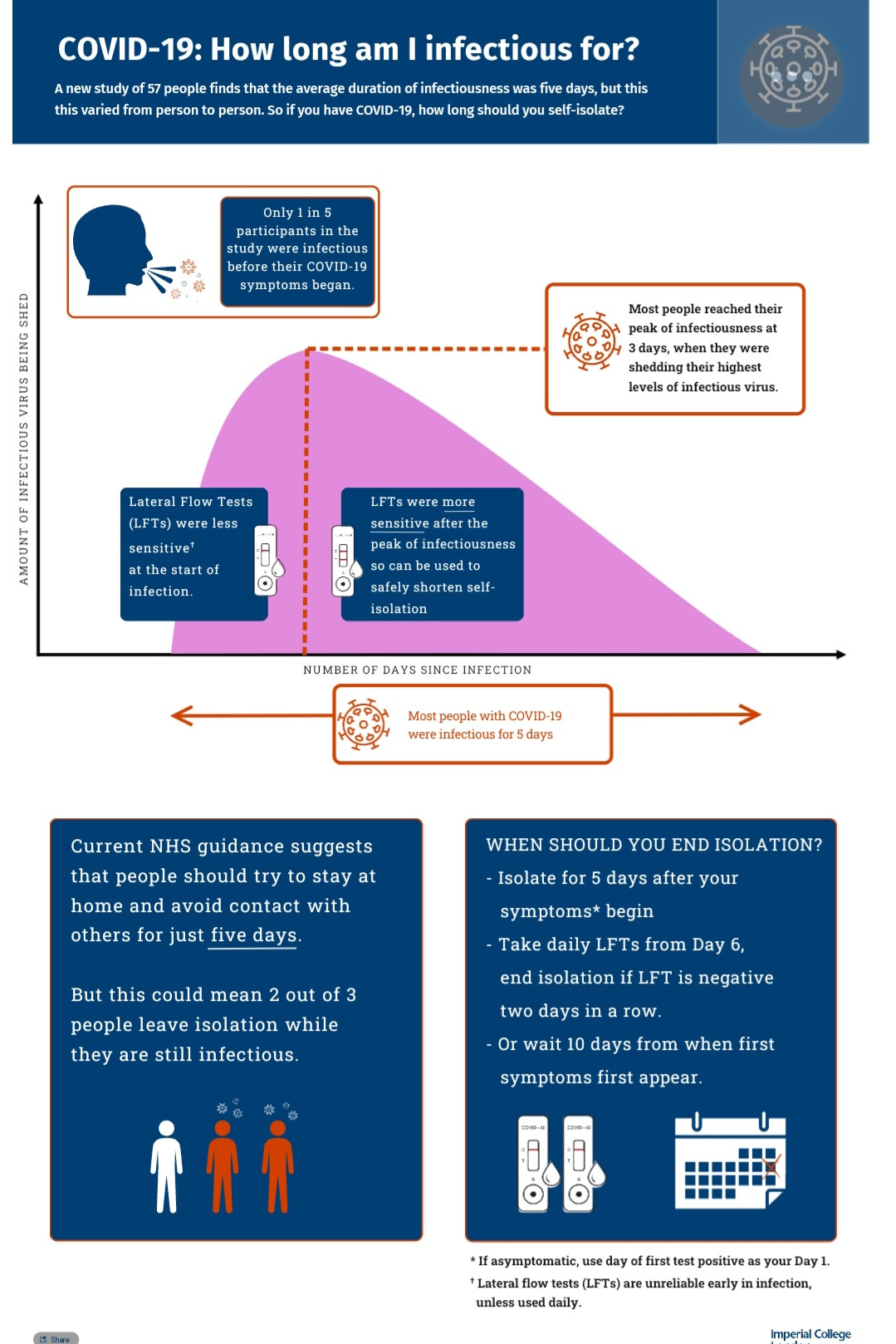
A real-world study led by the Imperial College London and published in The Lancet Respiratory Medicine journal found that in people who develop symptoms, the majority are not infectious before symptoms appear, but two-thirds of cases remain infectious five days after symptom onset. This was during earlier variants, but again confirming most people were still infectious on day 5.
These findings, along with numerous other studies, consistently indicate that individuals typically remain infectious for a minimum of 7 to 8 days, with a considerable number remaining infectious for 10 to 20 days.
A significantly more effective approach, rooted in scientific evidence, is outlined in the graphic above from the Imperial College of London. It suggests a protocol of isolating for 5 days followed by testing on day 6 to assess continued infectiousness. Repeat testing on day 7 helps confirm the results. If negative, it's likely that the individual is no longer infectious and can safely end isolation. However, if the test is positive, continued isolation is necessary.
Following isolation, it's recommended to use a quality N-95 or similar mask for an additional 2 to 3 days while interacting with family members or being in public spaces to further reduce the risk of transmission.
It's particularly crucial to highlight this approach in light of the recent CDC update on isolation guidance. The shift from the previously recommended 5-day isolation period to just 24 hours after a fever, without testing, lacks scientific basis and isn’t grounded in logic. It should be retracted immediately. Failure to do so could have detrimental effects on all levels of society.
2. Can we determine if someone is infectious by looking for symptoms?
No. Determining an individual's infectiousness based solely on symptoms may not be sufficient, as recent studies indicate. The report "Detection of SARS-CoV-2 RNA in exhaled breath and its potential for prevention measures" (Sept 2023) highlights that symptom severity may not accurately reflect viral load progression in exhaled breath. As stated in the study, "Symptomatic and asymptomatic COVID-19 patients exhale distinctive amounts of SARS-CoV-2 not necessarily correlating with symptom severity”. This suggests that asymptomatic individuals, who may show higher exhaled breath viral shedding, could be highly infectious despite the absence of symptoms. Thus, incorporating exhaled breath testing into infection prevention measures is crucial, as it can identify infectious individuals regardless of symptom presentation.
Furthermore, a study from August 2022 found that "the viral loads of asymptomatic and symptomatic patients did not differ significantly", indicating that relying solely on symptoms may not accurately differentiate between infectious and non-infectious individuals.
Supporting this, surveillance data from March 8, 2022, concludes that "Robust testing of asymptomatic people and rapid isolation and quarantine of members who are exposed or infected effectively limited the spread of SARS-CoV-2 during the Fall 2020 semester". These studies highlight the significance of including asymptomatic testing in containment efforts to effectively control the spread of COVID-19.
3. Is there evidence that shows SARS-Cov-2 spreads from school-age children to adults leading to the hospitalization of adults?
Yes. The New England Journal of Medicine published a study on July 21, 2021, in which over a dozen Ph.D.'s, MDs, and other officials from the CDC in Atlanta, the Georgia Department of Public Health investigated an outbreak. They wrote, " This retrospective study showed that the efficient transmission of SARS-CoV-2 from school-age children and adolescents to household members led to the hospitalization of adults with secondary cases of COVID-19." They said that two-thirds adopted physical distancing because of a known exposure and that it may have reduced some of the in-household transmission. Despite that, the transmission from school-age children to adults resulted in the hospitalization of adults. They conclude that " when feasible, children and adolescents with a known exposure to SARS-CoV-2 or a diagnosis of COVID-19 should remain at home and maintain physical distance from household members."
4. Is there evidence that SARS-CoV-2 is in the air and spreading within schools?
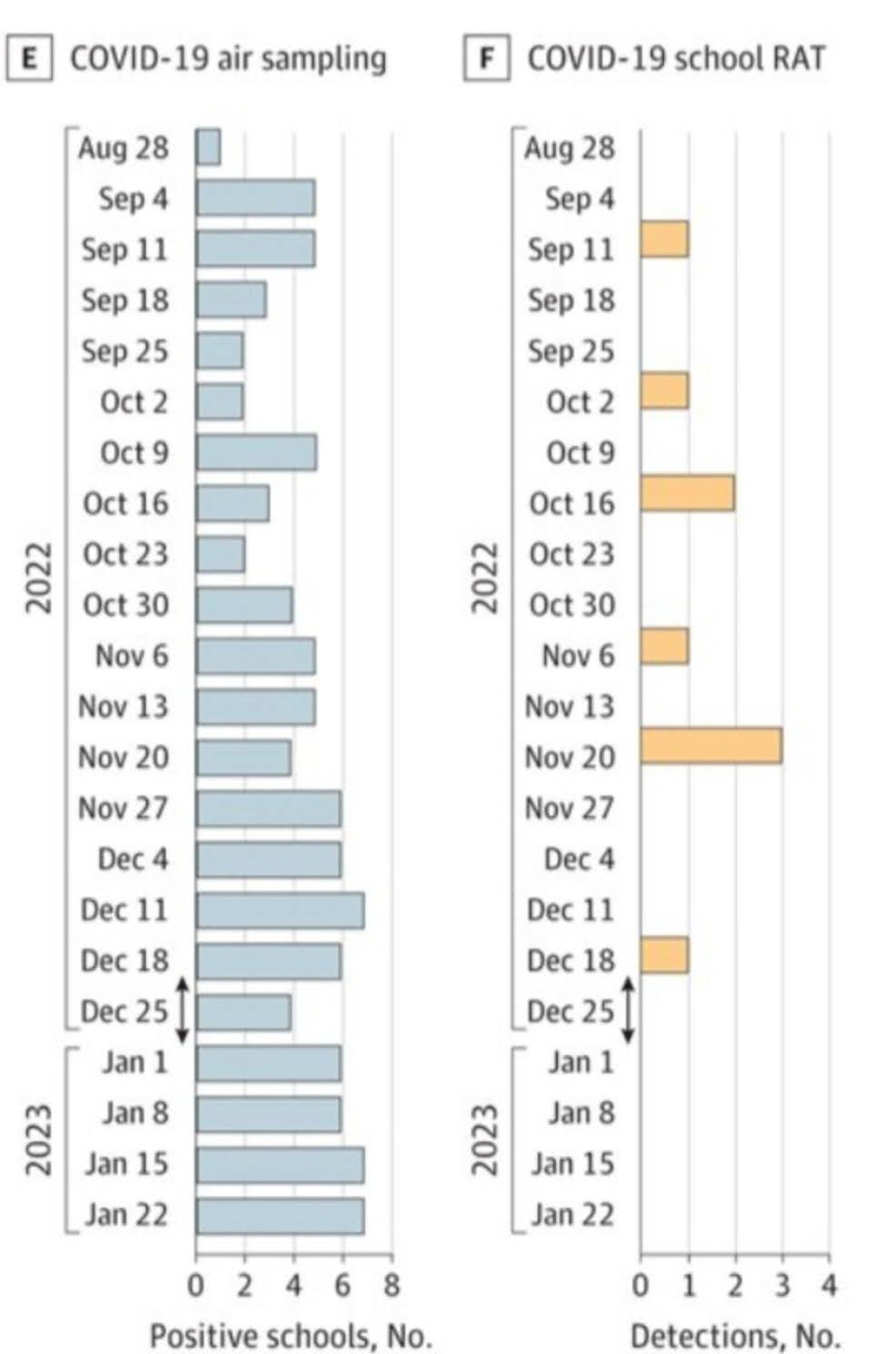
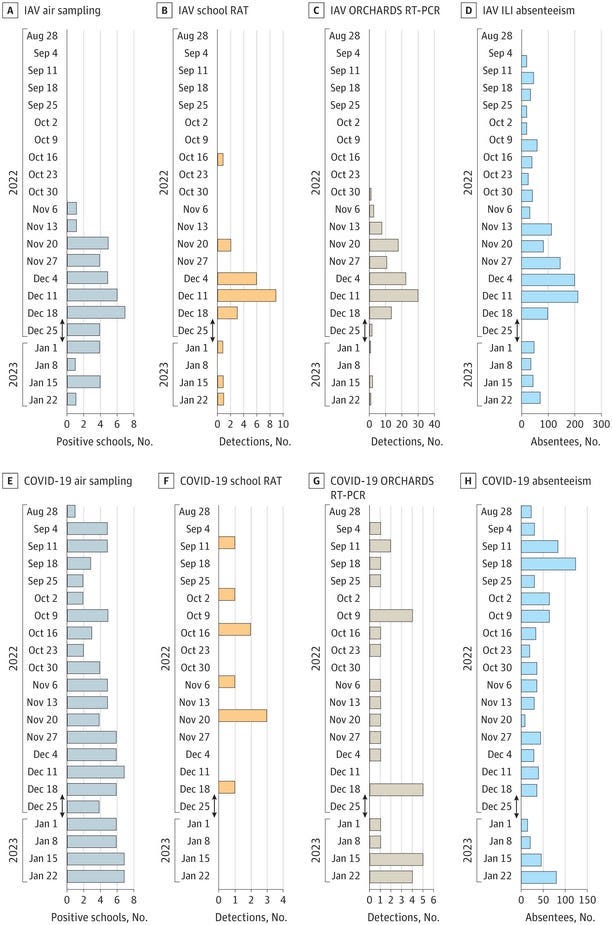
Yes. A study published on December 5, 2023, focused on air sampling, rapid antigen testing, and PCR testing, then compared that with absences. This shows the differences between testing methods and the prevalence of SARS-CoV-2 and influenza in the air across multiple schools in a school district in Wisconsin. This study reveals several alarming truths about the virus's silent spread and the limitations of current testing methods.
The study, conducted in Wisconsin schools, found that rapid antigen tests (RAT), the mainstay of at-home and school testing programs, are woefully inadequate. They often won't detect COVID until 4 to 5 days after exposure or symptom onset, which means they miss a significant number of infections while children are having the most symptoms. We can see this below.
The Rapid tests’ negative results within the first few days, when children and young adults are most severely impacted, create a false sense of security likely contributing to the continued spread of the virus.
The study's findings reinforce the need for comprehensive testing strategies that go beyond rapid tests to capture a more accurate picture of COVID-19 prevalence in schools.
Airborne Threat is Very High in Schools:
Utilizing air sampling technology, the study paints a disturbing picture of COVID-19's presence in the air of schools. The virus lingers in classrooms, hallways, and cafeterias, far exceeding the levels of influenza.
This widespread airborne transmission poses a significant health risk to students and staff, highlighting the need for automated ventilation that maintains CO2 at 600 ppm and air filtration systems that can filter out viral particles.
As shown in the graphic below, absenteeism attributed to the flu is showing up “before” influenza is found in the air. When a COVID test comes back negative from the school nurse, doctor, or at home, parents will often consider the reason for the absence to be the flu. This can be attributed to the rapid antigen tests producing a negative result. COVID is shown to be present in the air at the time of those absences.
Switzerland Air Sampling Study
If that doesn’t paint a clear enough picture, an earlier study published on May 16, 2023, conducted in Switzerland using air sampling, had similar findings. The study findings revealed alarming evidence of sustained airborne transmission of SARS-CoV-2 within schools. Molecular analysis confirmed the presence of the virus in aerosols and saliva samples, highlighting the urgent need for preventive measures.
According to the study, when it comes to reducing aerosol concentrations and curbing transmission, mask mandates surpass the effectiveness of air cleaners. With universal mask use in place, aerosol concentrations were 70% lower, and using air cleaners lowered concentrations by 40% on average. The researchers in the Switzerland study concluded, “Molecular detection of airborne and human SARS-CoV-2 indicated sustained transmission in schools.”
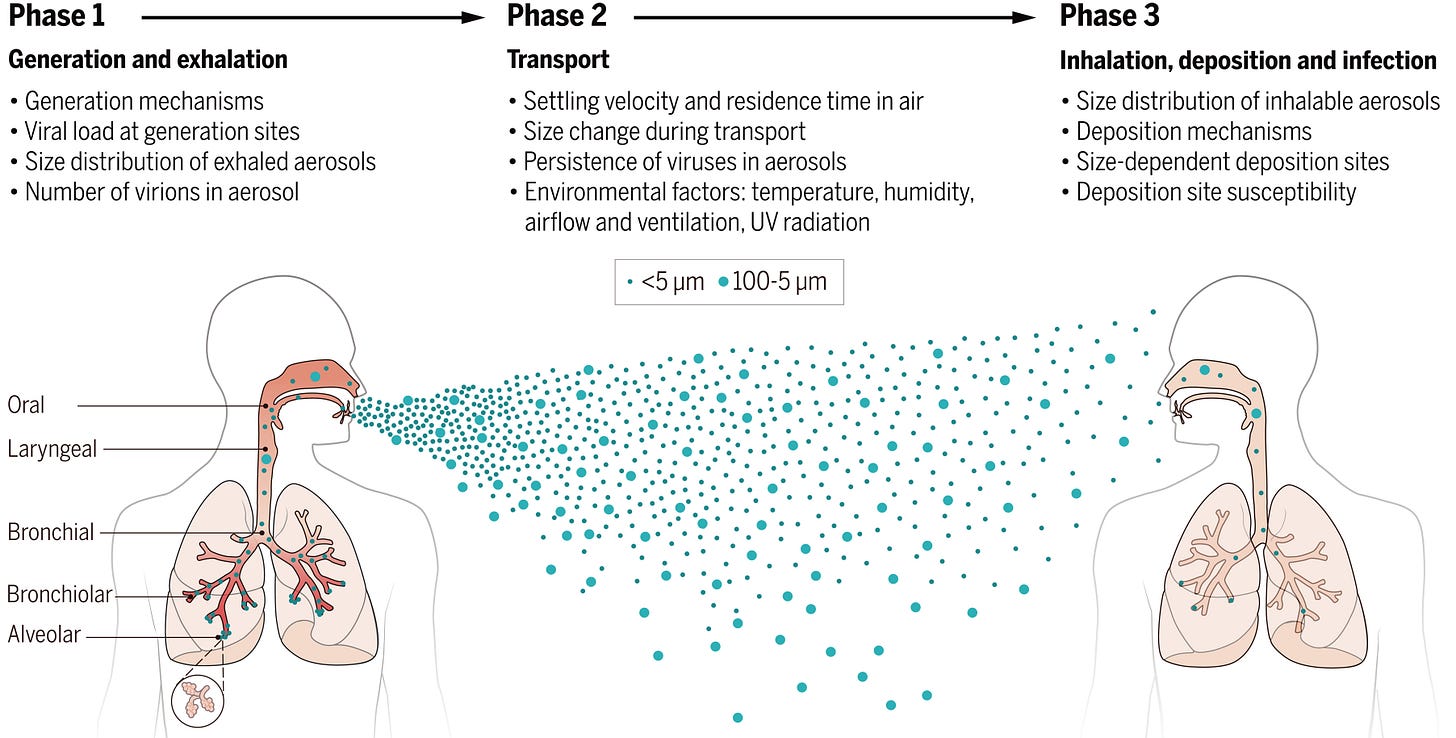
5. Do we have a better understanding of the mechanisms of airborne transmission of respiratory spread viruses and bacteria?
Yes. "The COVID-19 pandemic has highlighted controversies and unknowns about how respiratory pathogens spread between hosts. Traditionally, it was thought that respiratory pathogens spread between people through large droplets produced in coughs and through contact with contaminated surfaces (fomites). However, several respiratory pathogens are known to spread through small respiratory aerosols, which can float and travel in air flows, infecting people who inhale them at short and long distances from the infected person. Wang et al. reviewed recent advances in understanding airborne transmission gained from studying the spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and other respiratory pathogens. The authors suggest that airborne transmission may be the dominant form of transmission for several respiratory pathogens, including SARS-CoV-2."
"Aerosols produced by an infected individual may contain infectious viruses, and studies have shown that viruses are enriched in small aerosols (<5 μm). The transport of virus-laden aerosols is affected by the physicochemical properties of aerosols themselves and environmental factors, including temperature, relative humidity, ultraviolet radiation, airflow, and ventilation. Once inhaled, virus-laden aerosols can deposit in different parts of the respiratory tract. Larger aerosols tend to be deposited in the upper airway; however, smaller aerosols, although they can also be deposited there, can penetrate deep into the alveolar region of the lungs. The strong effect of ventilation on transmission, the distinct difference between indoor and outdoor transmission, well-documented long-range transmission, the observed transmission of SARS-CoV-2 despite the use of masks and eye protection, the high frequency of indoor superspreading events of SARS-CoV-2, animal experiments, and airflow simulations provide strong and unequivocal evidence for airborne transmission."(published in Science, August 27, 2021)
6. Do airborne viruses, particularly, COVID-19 lead to excessive absenteeism?
Yes. Preventable airborne viruses result in excessive absenteeism. We can see this in the study that utilized air sampling and tracked absenteeism in the Wisconsin school district.
On October 12, 2023, The non-profit advocacy group Attendance Works posted an article on the data they analyzed from the U.S. Department of Education, revealing that 66% of students attend schools with high or extreme levels of chronic absenteeism. There has been a doubling of the chronic absenteeism rate since before the pandemic, reaching 29.7% in 2022 from 16.2% in 2019. This crisis has affected over 14 million students, up from 8 million before the pandemic. High chronic absenteeism levels not only impact absent students but also affect everyone in the classroom, including teachers.
This issue places a significant burden on schools, making it difficult for teachers to meet the needs of all students, juggling efforts to catch up on absentees while keeping other students engaged. In the 2021-22 school year, they showed that 43% percent of schools had extreme levels of chronic absence. “Elementary schools were especially affected with extreme chronic absence jumping from 7% to 38% of all elementary schools.”
Immunity Debt Theory is Unsupported by Scientific Evidence
Just in case someone is reading this who still believes in the “Immunity debt” theory, consider this: babies born after the COVID-19 mitigation measures ended are suffering elevated rates of invasive Group A Strep (iGAS). A study from May 2023, now accepted for publication in Family Medicine and Community Health Journal, implicates the role of prior COVID-19 infections in the surge of severe RSV cases in young children.
The notion that 'immunity debt' is responsible for these concerning health impacts is merely a belief, unsupported by scientific evidence. If exposure to numerous pathogens indeed strengthened immunity, we would expect children throughout the past millennium to have enjoyed robust health. it wasn't until the advocacy for implementing public health measures that we witnessed significant improvements in children's health, less chronic illness, and life expectancy increase.
What This Means For How We Protect Children and Society
With mounting evidence of airborne transmission of numerous respiratory viruses, it's imperative to recognize that airborne transmission is far more common than previously assumed.
In light of our evolving understanding of COVID-19, it's imperative to reevaluate the significance of aerosol transmission in all respiratory infectious diseases. It's crucial to implement additional precautionary measures aimed at mitigating airborne transmission, both at short and long ranges. This includes prioritizing factors such as maintaining ventilation through automated systems ensuring CO2 remains below 600 ppm, considering airflows, and increasing air filtration to remove pathogens, including viral particles, from the air. When appropriate, ensure the use of properly fitted N-95 or similar quality masks.
These interventions serve as indispensable tools in significantly reducing transmission rates within various settings, including schools, hospitals, homes, and other indoor spaces. By doing so, we can better safeguard the health of children and individuals, mitigating the potential for chronic health issues caused by these airborne pathogens.
It's essential to recognize that COVID-19 alone can lead to a myriad of long-term health complications, resulting in unnecessary suffering and financial hardship. COVID-19 can weaken immune systems and increase the risk of secondary infections. Coinfections with other airborne viruses and bacteria often result in more severe outcomes. Therefore, proactive measures to address airborne transmission are critical in protecting public health and preventing the adverse impacts associated with COVID-19 and other respiratory infections.
The choice is clear: prevention now or grappling with the aftermath later. This is not just a health crisis; it's a societal threat that eventually jeopardizes every facet of life.
Now is the time for decisive leadership. The responsibility lies with each of us to safeguard the well-being of our communities and secure a healthier, more resilient future, but we need leaders who recognize the threat COVID imposes and proactively educate the public while diligently working to protect our schools by creating a sustainable path forward that doesn't leave anyone behind. It's crucial to upgrade ventilation and filtration systems, along with updating policies and procedures, to effectively mitigate the transmission of COVID-19 and other airborne pathogens.
Let our actions today shape a safer and healthier tomorrow. We must work Together Against COVID Transmission.
Please share your thoughts and let us know how COVID-19 is impacting you or anyone you know. Share stories of how COVID has impacted your children. Share questions that weren’t answered here.
You can join us in advocating for Clean Air for Kids by taking action Here.