BA.2.86 with two additional mutations is responsible for U.K. care home outbreak and it had an 86% Attack Rate! How could this impact the latest boosters?
What do we know about BA.2.86? What can Japan hospitalizations tell us about what to expect?
BA.2.86 (Pirola) variant with two additional mutations is the cause of a U.K. care home outbreak. It had an 86% attack rate. The studies on this variant showed immune evasion the likes of which we haven’t seen before. They also showed a lower infectivity than EG.5.1, which is currently dominating and growing in prevalence. There are several variants gaining in prevalence at this time. HV.1 is another that the CDC variant proportions shows is gaining ground. The number of variants spreading is higher than at any other time and that is exactly what this virus wants. This gives it more opportunities to mutate and evolve around anything we throw at it. As far as BA.2.86 with two new mutations that rapidly spread through a care home in the U.K., the good news is that only 1 person was hospitalized, and there were no reported deaths, as of yet. The concern is that the new mutations gave it an advantage to become much more infectious and that persisting in people instead of hospitalizing them is exactly what the virus wants. Persisting in people gives it an advantage, but it causes many long-term problems, reducing the quality of life and ultimately shortening lifespans.
In the U.K. SARS-CoV-2 variant surveillance and assessment: technical briefing 53, they discuss what they know about BA.2.86.
They say the following,
Situational assessment BA.2.86 (Variant Technical Group of 5 September 2023)
There is a continued slow accumulation of cases globally including cases reported from new countries. The rate of detection of new sequenced cases cannot be used as an indicator of growth due to limited and lagging genomic surveillance globally.
BA.2.86 is now more globally dispersed than other lineages of similar age in 2023. This may have been the result of international seeding from one or more unknown sources through mass travel. However, with apparent established transmission chains now in many countries, these seeding events are now unlikely to be the key driver of spread.
The data suggest established community transmission of BA.2.86 within the UK. This is based on the detection of multiple unlinked cases in different regions of the UK, without identified travel links, and phylogeny (the relationship between cases as determined by viral genomic data). This finding does not confirm that BA.2.86 has a growth advantage within the UK compared to other circulating variants.
A single care home outbreak was investigated due to a high attack rate and found to be BA.2.86. This cannot be used to make an assessment of the variant’s fitness but in contrast to recent laboratory data suggesting lower infectivity in vitro, this is an early indicator that the variant may be sufficiently transmissible to have impact in close contact settings.
Pseudovirus neutralisation data is available from several laboratories. Whilst this data has limitations, antigenic cartography based on mouse sera is mostly consistent with the antigenic distances estimated from the mutational profile. The potential UK population impact after several vaccines and waves cannot be extrapolated from the available data.
Some early indicators of increasing COVID-19 transmission in the UK were noted and behavioural, immunological and virological factors may all be contributing. We cannot confirm that BA.2.86 is contributing to any increase given available data.
There is an insufficient number of cases to make an assessment of outcome or severity. In the UK, the current surveillance systems do not support an assessment of comparative severity between variants but trends in severity and outcomes can be monitored over time through hospital data. It is likely that any such signal will take weeks to be visible and confirmed through sequencing.
Regarding the care home outbreak they lay out the following details. “As of 5 September 2023, 33 out of 38 residents have tested positive for SARS-CoV-2 (attack rate 86.6%). Of the 33 positive residents, 19 (57.6%) were symptomatic with symptom onset between the 20 August 2023 and 28 August 2023; 29 of the residents have now recovered, while 4 remain unwell. One resident was hospitalised as a result of their illness (hospitalisation rate, 3.0%), and no deaths due to COVID-19 have been reported. Twelve staff tested positive either by LFD and/or PCR, and all have now recovered. No staff members were hospitalised.”
The good news is that there weren’t any deaths and only one was hospitalized. The question is, how many will have persistent infections and new onset of chronic conditions? The persistent infections are allowing COVID to adapt around any new treatments by mutating within the person taking treatments.
Bases on the available data, BA.2.86 (Pirola) is expected to cause more persistent infections and immune suppression, which will likely also lead to secondary infections. How many will die of "other" causes in the near future? Will that data ever be released?
According to the latest data, BA.2.86 evades all monoclonal antibodies and antibodies from XBB infections and/or vaccines. Moderna claims that their vaccine is effective against severe disease and death and if that is true then it is only mildly helpful to the vast majority of people because the vast majority of people won’t experience severe disease or death if infected. The vast majority of people do have to worry about the damage an acute infection causes, the time lost from work and school and the very real risk of the virus persisting in different tissue throughout the body, leading to autoimmune disorders, vascular dysfunction, cognitive and neurological dysfunction and other longer term chronic health conditions.
There is a new study on COVIDs ability to persist long after the initial infection.
“SARS-CoV-2 reservoir in post-acute sequelae of COVID-19 (PASC)”
(Published Sept 4 2023)
Abstract
"Millions of people are suffering from Long COVID or post-acute sequelae of COVID-19 (PASC). Several biological factors have emerged as potential drivers of PASC pathology. Some individuals with PASC may not fully clear the coronavirus SARS-CoV-2 after acute infection. Instead, replicating virus and/or viral RNA—potentially capable of being translated to produce viral proteins—persist in tissue as a ‘reservoir’. This reservoir could modulate host immune responses or release viral proteins into the circulation. Here we review studies that have identified SARS-CoV-2 RNA/protein or immune responses indicative of a SARS-CoV-2 reservoir in PASC samples. Mechanisms by which a SARS-CoV-2 reservoir may contribute to PASC pathology, including coagulation, microbiome and neuroimmune abnormalities, are delineated. We identify research priorities to guide the further study of a SARS-CoV-2 reservoir in PASC, with the goal that clinical trials of antivirals or other therapeutics with potential to clear a SARS-CoV-2 reservoir are accelerated."
Moderna’s statement on the efficacy of its new vaccine against BA.2.86, without the two additional mutations, says the following. “Moderna, Inc. announced that clinical trial data from its research assay confirm its updated COVID-19 vaccine, which is pending approval by the U.S. Food and Drug Administration for the fall 2023 vaccination season, generates an 8.7-fold increase in neutralizing antibodies in humans against BA.2.86 (Pirola), a variant under monitoring. The Centers for Disease Control (CDC) indicates that the highly mutated BA.2.86 variant may be more capable of causing infection in people who previously had COVID-19 or were vaccinated with previous vaccines, noting that updated COVID-19 vaccines may be effective in reducing severe disease and hospitalization.”
They don’t say if that increase in antibodies prevented infection or how long that increase lasts. Based on the data from the prior booster, the antibodies do not last long at all. Anywhere from one to three months. They couldn’t know what any additional mutations will do to their data. Read more on the bivalent booster risks because many of the same risks apply to this new booster. “Important Booster Considerations.”
Yunlong Richard Cao, a Harvard educated professor studying biochemistry and immunology, studied BA.2.86 impact on antibody neutralization and the mutations, stated the following on X. His handle is @Yunlong_Cao
1) BA.2.86 is antigenically distinct compared to XBB.1.5.
2) BA.2.86 can significantly escape XBB-infection/vaccination induced antibodies.
3) However, the infectivity of BA.2.86 may be much lower than XBB.1.5 and EG.5.
“By using pseudovirus neutralization assay and antigenic cartography (based on mRNA immunized mouse serum), we found that BA.2.86 is antigenically distinct from WT, BA.2, BA.5, and XBB.1.5. This means that XBB-induced antibodies cannot well recognize and neutralize BA.2.86.”
“Results showed that N450D, K356T, L452W, A484K, V483del, V445H are the key mutations responsible for BA.2.86's enhanced immune evasion than XBB.1.5.”
“In sum, we found that BA.2.86 is antigenically distinct from XBB.1.5 and can escape XBB-induced neutralizing antibodies. The updated vaccine's efficacy against BA.2.86 should be closely monitored; however, BA.2.86 may not prevail very fast due to its lower infectivity.”
This was before the news out of the U.K. on the additional mutations and the 86% infection rate in a care home. It appears that BA.2.86 has figured out how to increase the infectivity with these two additional mutations.
In other words, we are dependent on our finite supply of T-cells. The lower the viral load exposed to, the longer we live, and the better the chance we have to avoid a persistent infection.
A very concerning issue is that the latest vaccines won't likely offer much benefit to the majority of people, if any. They may help boost T-cell immunity if someone hasn't been recently infected, but according to the latest data, BA.2.86 already evades XBB.1.5 antibodies, so once again, the vaccine makers are falling short of the viruses ability to out maneuver the immune response.
The Sato Lab (@sytemsvirology on X) said, “Three monoclonal antibodies (Bebtelovimab, Sotrovimab, Tixagevimab) that were antiviral against the parental BA.2 (see the G2P-Japan 9th paper) did NOT work against BA.2.86 AT ALL"
The Sato Lab went on to conclude, “Altogether, it is suggested that BA.2.86 is one of the most highly immune evasive variants ever and should have the potential to be considered as a variant of interest."
As of now, we don’t know if this impacts the efficacy of Paxlovid so we will have to watch for that but at this time, Paxlovid is the best viable treatment approved to fight a COVID infection and it often isn’t made available to people. If cases surge then millions that need it may not be able to get it.
What can Japan hospitalizations tell us?
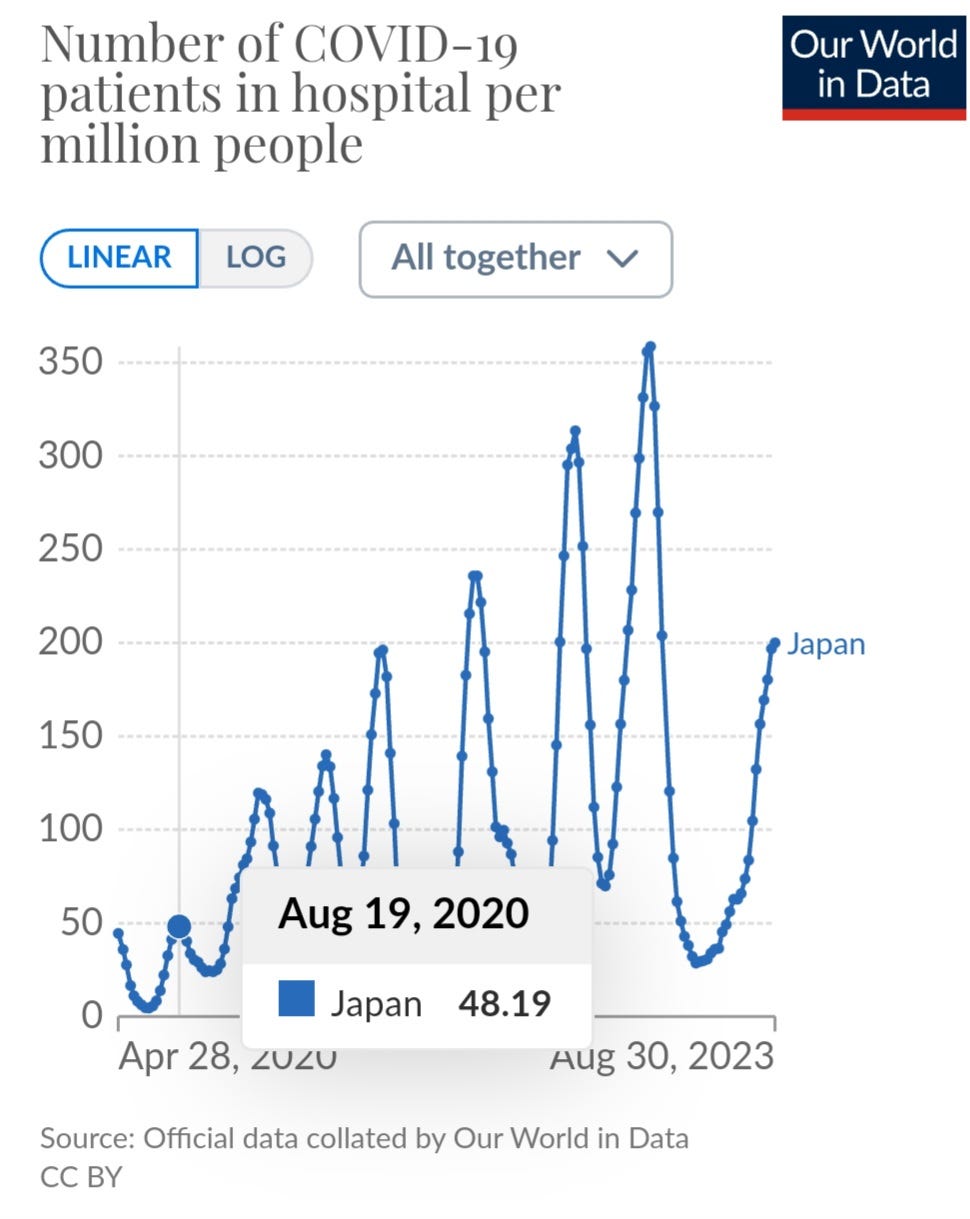
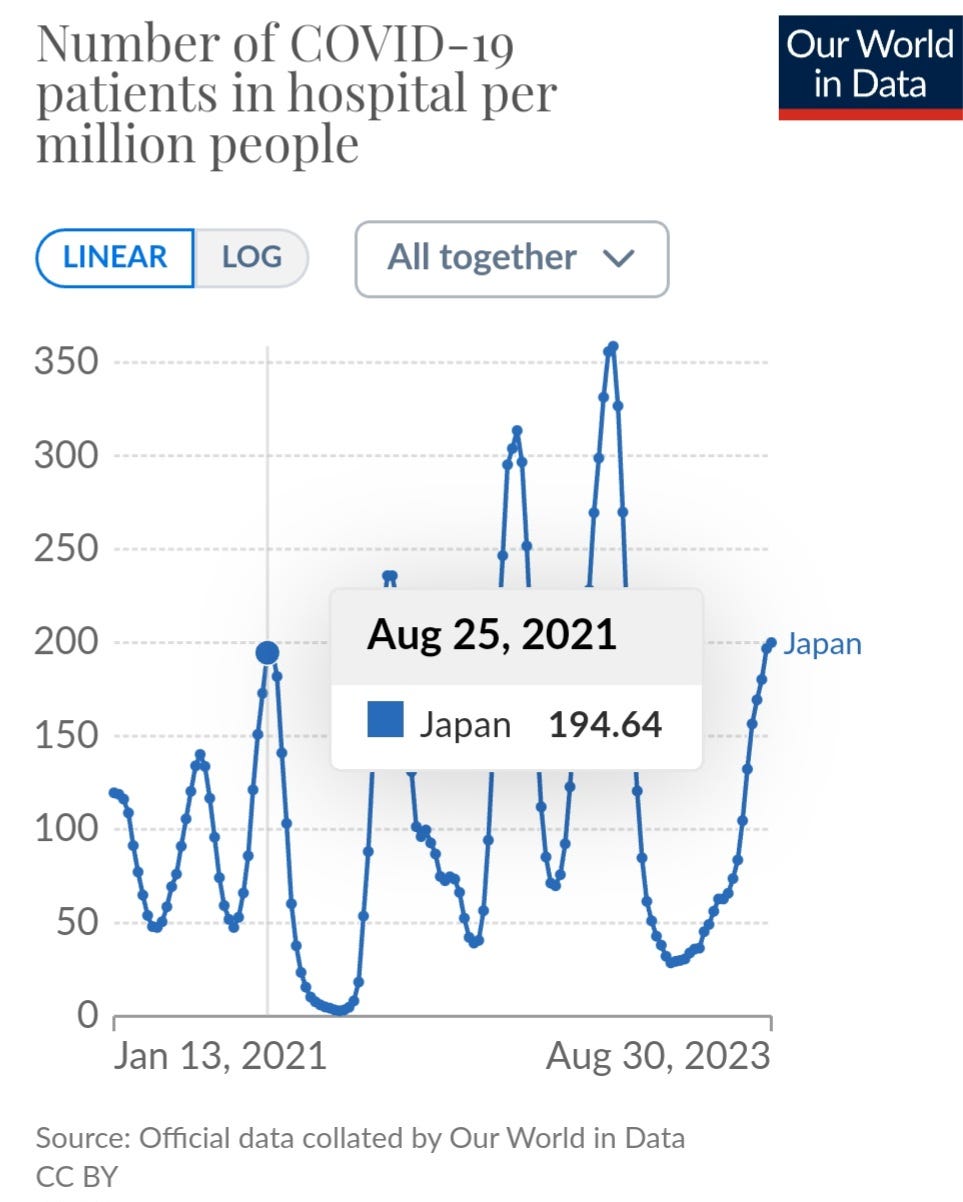
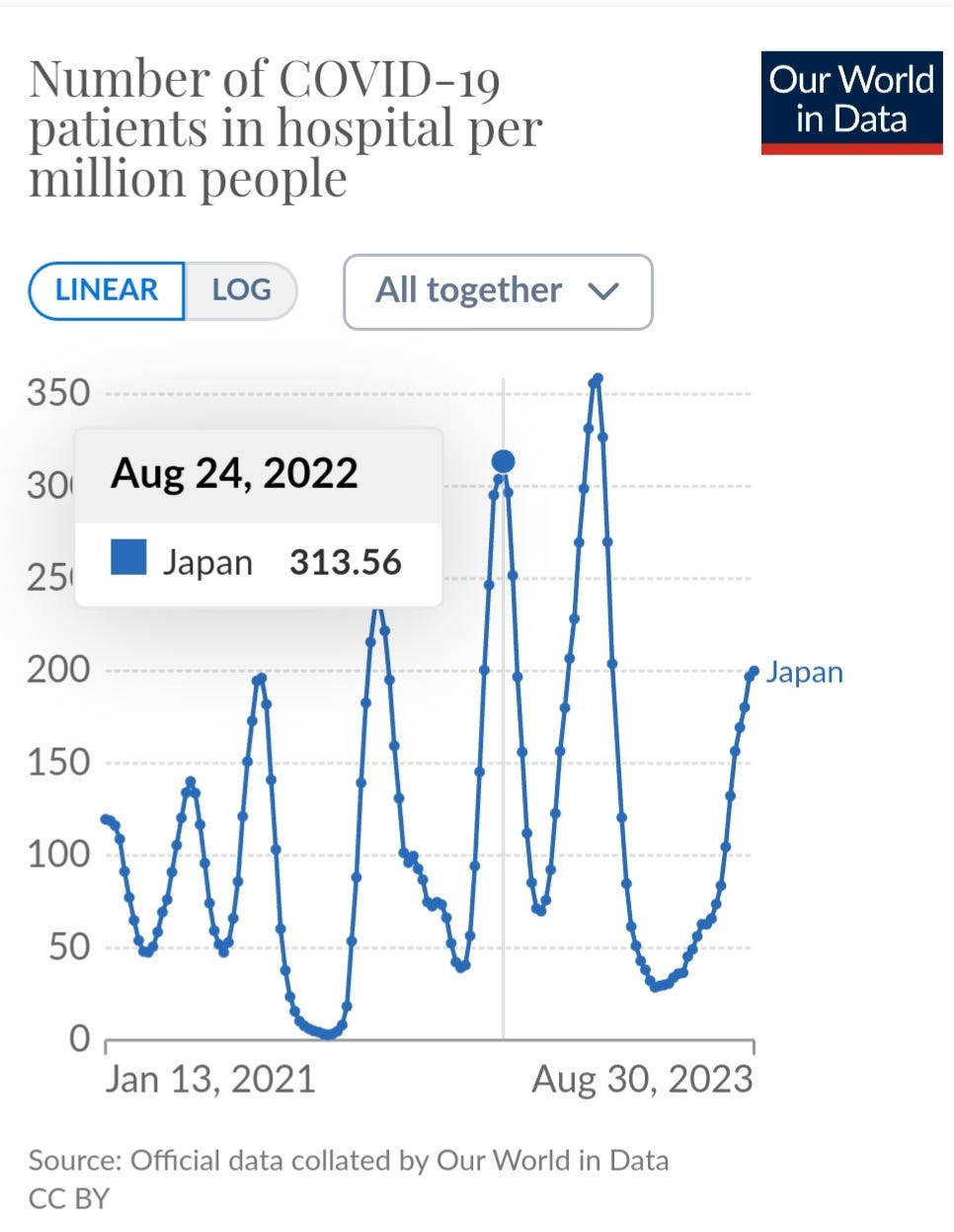
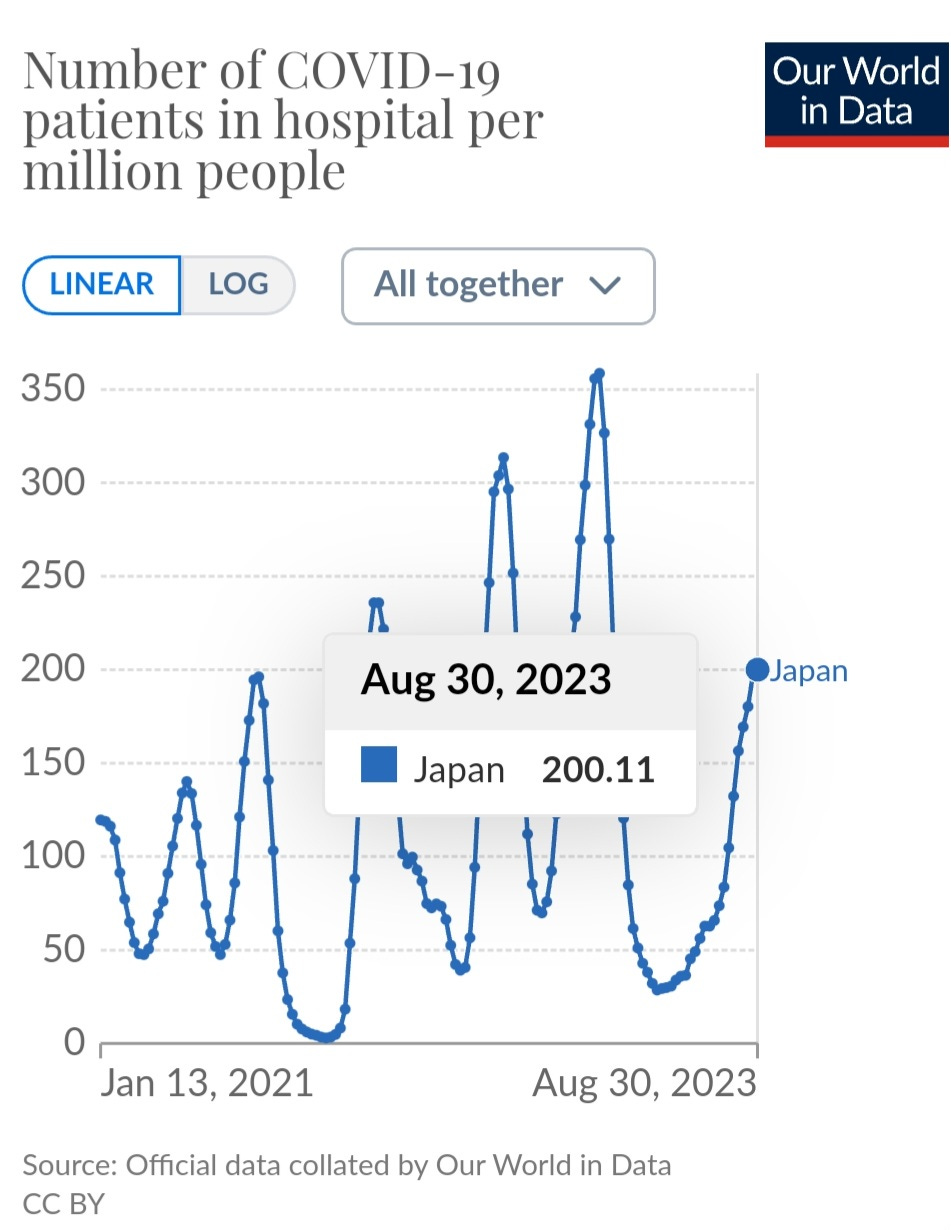
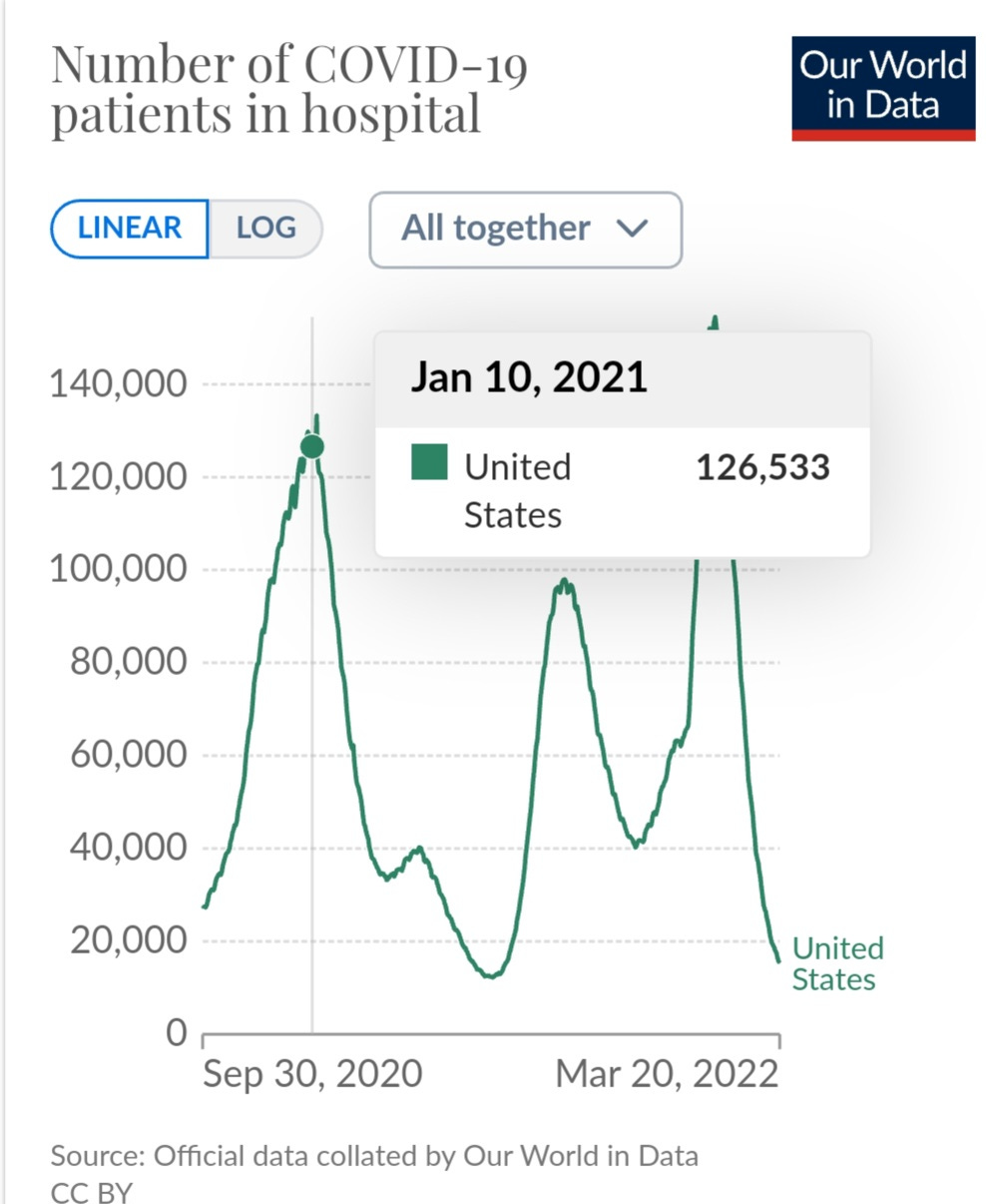
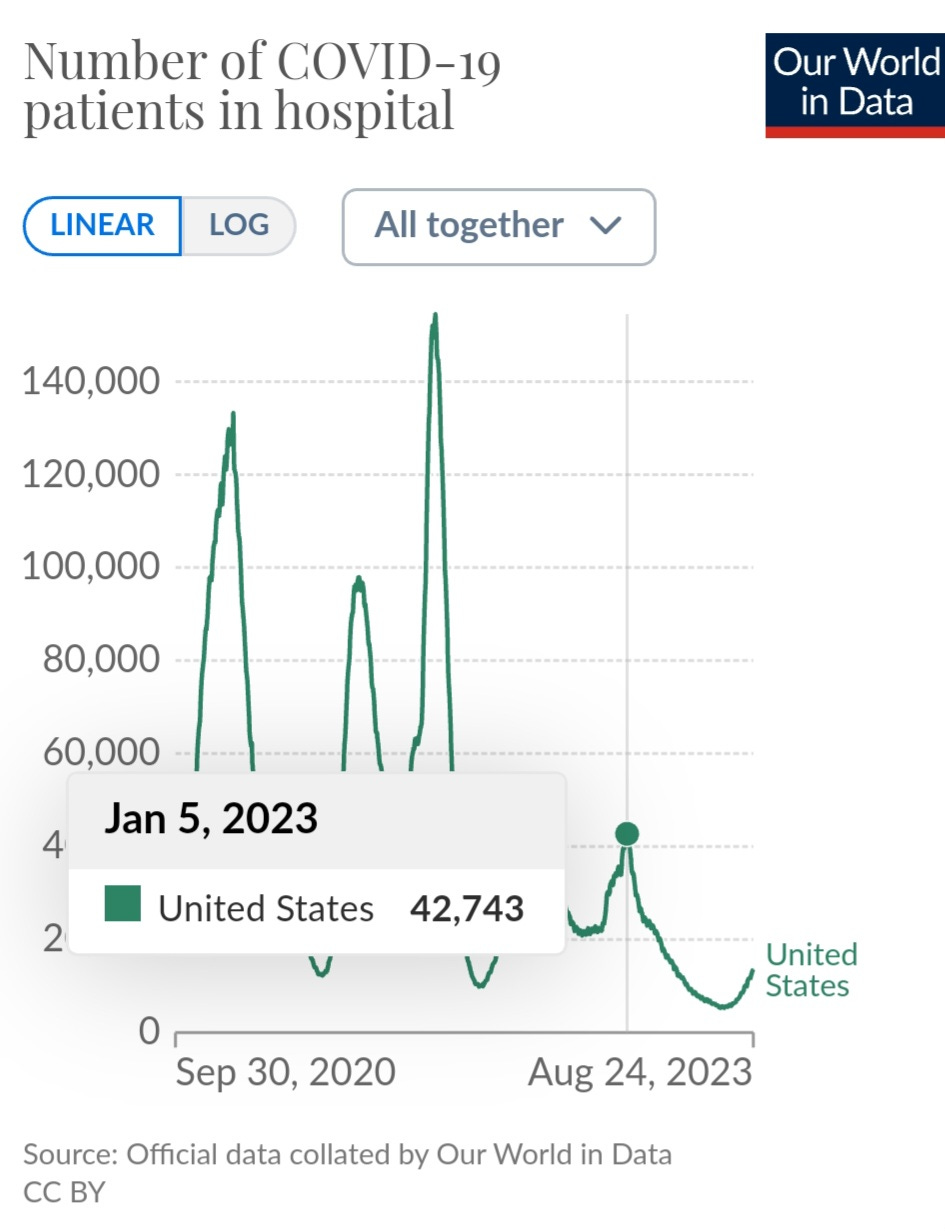
For the third straight year, COVID hospitalizations appear to have peaked toward the end of August. In 2020, it peaked a little earlier because there were a lot of mitigation measures in place slowing down the exponential growth between schools and homes and into the general community.
It looks like Japan hospitalizations will peak around the 2021 level.
Schools close in Japan around July 20th for summer break. It isn't a coincidence that hospitalizations peak 2 to 4 weeks later. Schools closing stopped the exponential growth between classrooms and homes, students to siblings, and then to new classrooms. Along the way spreading to parents, coworkers, and up through the age groups.
Now, lets consider the new mutated BA.2.86 that ripped through the care home in the U.K. What will an 86% SAR (Secondary Attack Rate) mean for schools once this variant takes old in schools. It means that a peak of exponential growth in January has the potential to match or surpass the first Omicron surge.
How do we know it will peak in January?
It isn’t a coincidence that 2 to 4 weeks after U.S. schools close for winter break we see hospitalizations peak, just like in Japan.
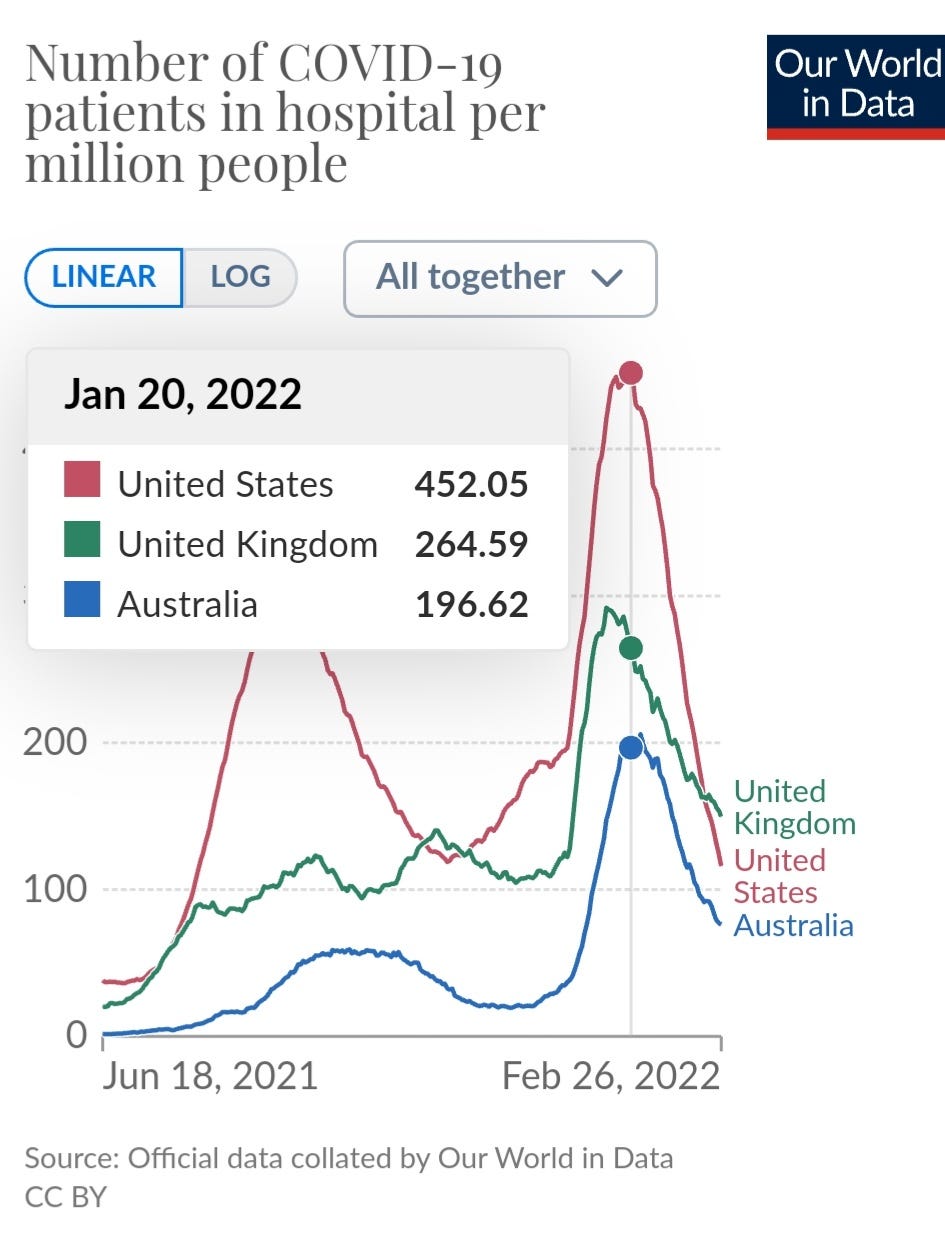
In case that isn’t convincing enough, what are the odds of multiple countries having the peak of hospitalizations around the same time in January?
Let’s add in different hemispheres as well.
Different mitigation measures at different times but in countries that have a holiday break at the same time. How could the peak happen at almost the same time? When you dig into it, the date of school closing and the mitigation measures in place shorten or extend the date hospitalizations stop increasing. If you have transmission gaining momentum between classrooms and homes as prevalence builds it takes two to four weeks for infections to get severe enough that hospitalization is required. Once the exponential growth is cut off then within two to four weeks we see exponential decay. This has been consistent all around the world. The transmission between classrooms and homes is the likely driver of exponential growth.
By implementing the level of mitigation protections that significantly limit the transmission of COVID-19 and other respiratory spread pathogens we could have a direct impact on the number of people hospitalized, the number of people that will suffer with Long-COVID and the number of people that will die. This is predictable. This is preventable.
Why aren’t people understanding this connection?
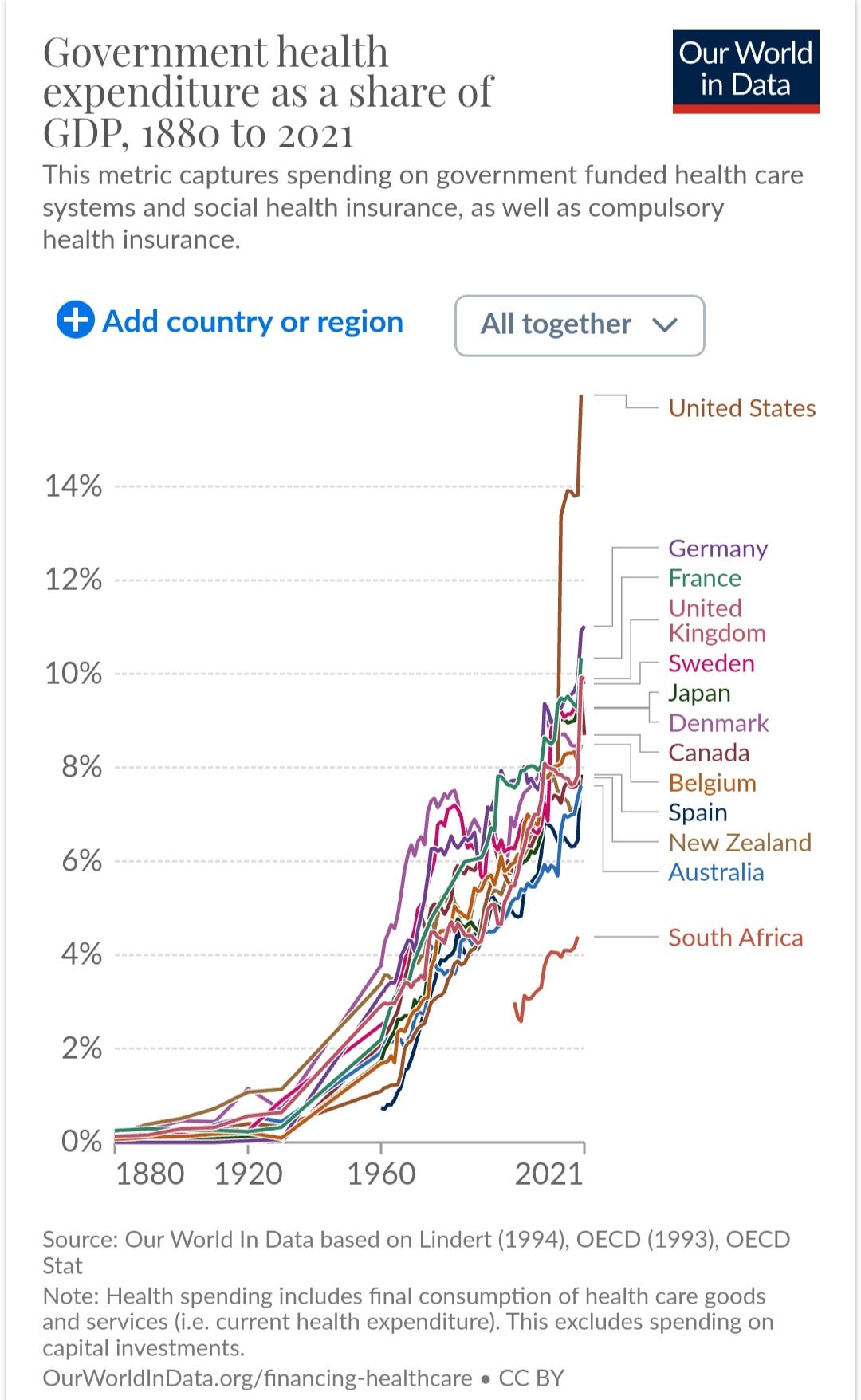
There are several reasons. First is the delay in time from when schools close until hospitalizations start decreasing. We have been told the increase is because people travel for the holidays but we can clearly see the exponential growth started way before the holidays. Another reason is that people don’t want to believe this is happening despite knowing their whole lives that children come home sick with flu, RSV and many other viruses and bacterial infections. There has been a disconnect as to how viruses like EBV and Varicella (chicken pox) often impact our lives decades later. By monitoring CO2, testing the wastewater, increasing ventilation and filtration and when necessary ask people to wear high quality N-95 or similar masks then we could live with this virus. Pretending it isn’t dangerous or that children aren’t spreading viruses ignores all the science and data. We are on an unsustainable path. The economy gets hurt. The overall cost of healthcare increases even more. According to the latest long COVID study, “Estimates place the total US economic cost of PASC at approximately $743 billion per year, including reduced quality of life, lost earnings and increased medical spending."
We can protect the health, quality of life and the longevity of people while bringing down expenditures on healthcare. That money can be invested in schools and towards the betterment of individuals lives. Billions of people could have a better quality of life if we simply understood that providing Clean Air for Kids is an absolute essential thing to do to secure that future.
We must work Together Against COVID Transmission in schools. Children are not immune to the long term chronic health issues caused by viral persistence. Further, children sitting in a classroom for extended periods of time are exposed to higher viral loads making infection more likely and making it harder for the body to fight off the virus. COVID has become more immune evasive and suppressive than ever before, making persistent infections and secondary infections much more likely. When the immune system takes a hit trying to fight off this disease children and their parents become more vulnerable to infection from other pathogens. If COVID gets into the areas of the body that it can remain and persist then that leads to autoimmune disorders, and other chronic health issues. This is predictable and more importantly, it is preventable.




10 cases of BA.2.86 in Denmark plus also found in wastewater in areas where the 10 cases didn't live, so it is already widespread and gaining ground in Denmark. This also shows that it is spreading globally. Still low numbers but definitely something to watch closely. Also, the 10 cases didn't have severe symptoms. That isn't the biggest concern, though. The biggest concern is immune evasion/suppression and its ability to persist, leading to long-term health issues.
With that said, a highly contagious and extremely immune evasive and suppressive variant can open the door to secondary infections and still hospitalize and kill a lot of people.
Conclusion of report:
"Given the widespread distribution of BA.2.86 globally and within Denmark in clinical samples and in wastewater, and the high number of mutations conferring immune-evasive potential, the possibility that BA.2.86 will outcompete currently dominating variants cannot be ruled out. Our very early clinical data suggest a clinical picture in line with the typical COVID-19 illness caused by previous variants. Data are presently very preliminary, and further global monitoring of BA.2.86 and other SARS-CoV-2 variants is highly warranted."
https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2023.28.36.2300460
Hi TACT...Glad you're still out there screaming into the void.
Thought you might like to take a look at the attached report from the European Union on the outbreak of BA.2.86 in Denmark.
One sentence I found of particular interest.
"ALL (cases) aged 18 years or above had been vaccinated against COVID-19 AT LEAST three times" (emphasis mine)
ALL victims vaccinated AT LEAST 3 times.
Curious that.
https://www.eurosurveillance.org/content/10.2807/1560-7917.ES.2023.28.36.2300460