COVID Update May 6, 2024: KP.2 Variant Challenges Past Infections and Vaccines as it Becomes The Top Variant, Symptoms, and the Summer COVID Forecast
Asymptomatic and Mild Infections Can Lead to Long Term Health Problems
Brace yourself: COVID-19 isn't slowing down. New variants are emerging at a terrifying pace, each more adept at evading our immune defenses. Mutations are piling up, not just on the spike protein, but deep within the virus's body, suggesting that it is evolving to evade or attack the immune system and other cells in different ways. KP.2 has risen to the top as predicted.
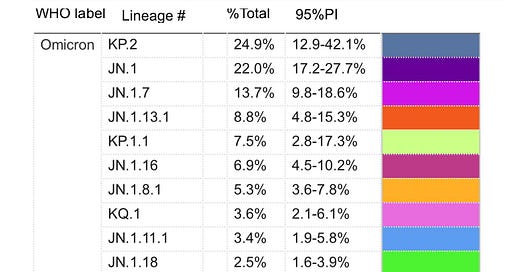
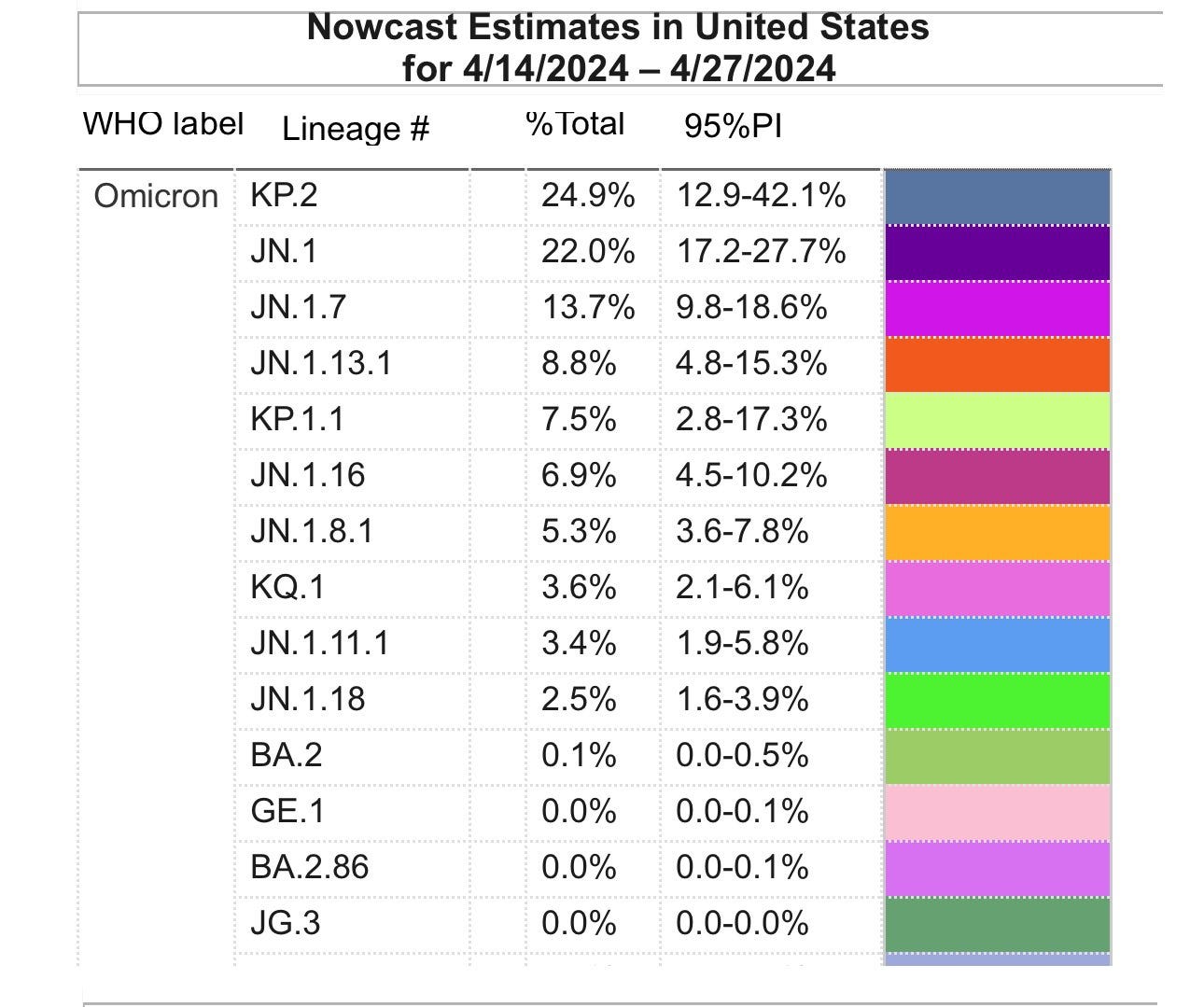
We can see that JN.1.16 and JN.1.13.1 are also increasing but these are likely increasing due to their offspring. JN.1.16.2 and JN.1.16.2.1, which has been shortened to LA.1, and JN.1.16.2.2 has been shortened to LA.2. Each of these is gaining momentum with LA.2 having the higher growth advantage.
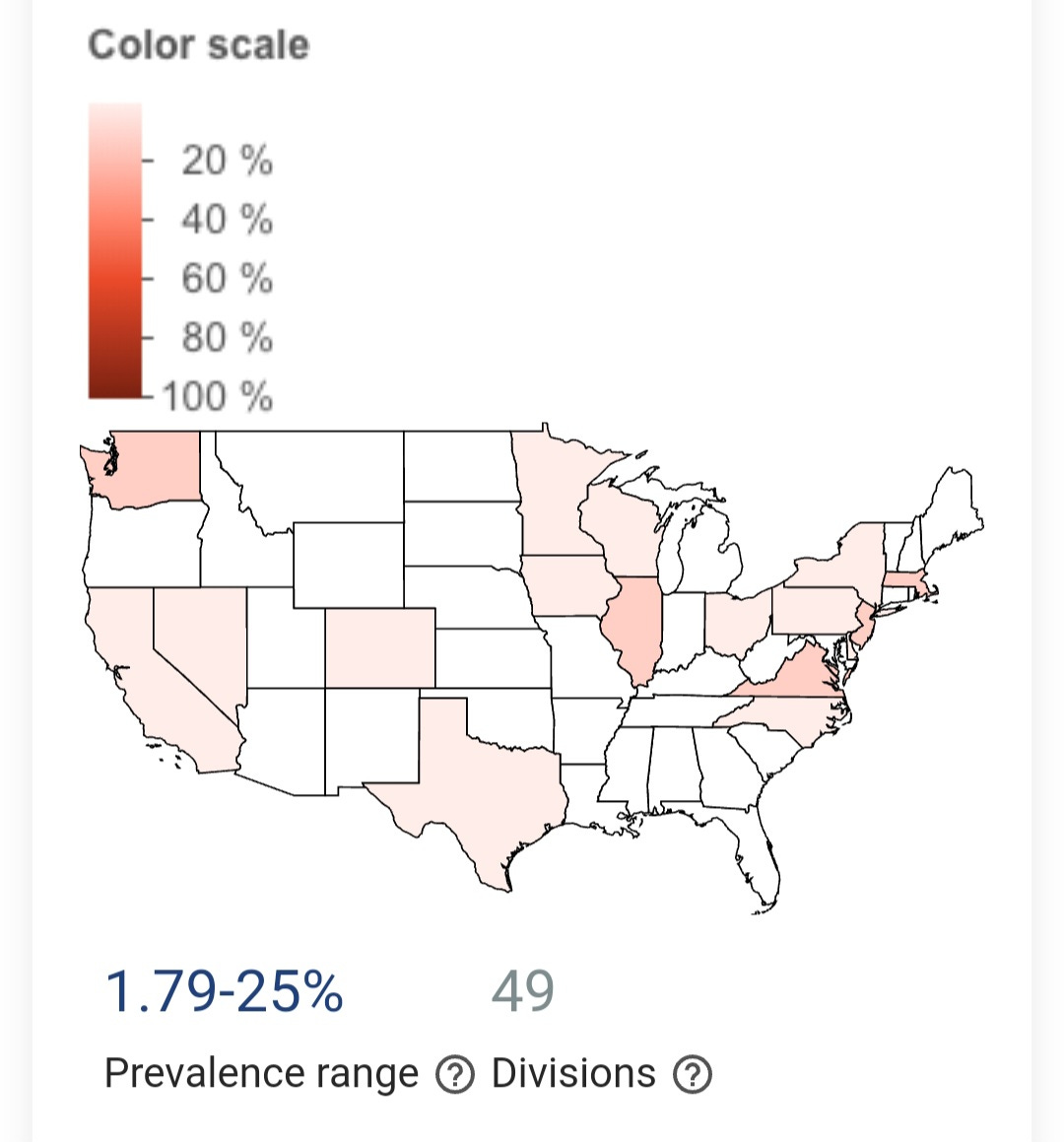
KP.2 in the U.S.
Don't be fooled by states where KP.2 seems absent. Many of the states barely test for new variants. This means KP.2 and others could be lurking undetected. We need better monitoring everywhere to get the full picture.
TACT’s March 16th update cautioned, “We have little reason to believe that KP.2 won’t further reduce the short-term efficacy of the XBB.1.5 targeted vaccines or that induced by prior XBB infection or even a JN.1 infection.” On April 26, 2024, the first study on KP.2, which we’ll go into in more detail below, shows us that KP.2 has evolved to further degrade vaccine efficacy and the natural immunity built from previous infections. This underscores the growing threat of persistent infections and the looming risk of Long COVID, even among those with very mild symptoms. We’ll list the symptoms to look out for as KP.2 becomes more prevalent and discuss asymptomatic infections.
We’ll look at the situation from a global perspective. Disappointingly, the W.H.O. has buried the latest SARS-COV-2 data into a May 1, 2024 report on influenza. We’ll provide an updated variant watchlist that continues to expand. We’ll also see which variants are surging in Canada. There are some surprises there. Finally, TACT’s overview will discuss the current situation and this summer’s COVID forecast.
Stay Informed, Stay Empowered: Independent Coverage
By subscribing, you'll gain access to:
Unbiased reporting: We cut through the noise and deliver critical information you need to make informed decisions about your health.
In-depth analysis: TACT goes beyond headlines to uncover details and the true impact of COVID, Bird Flu, Monkeypox, and other emerging or evolving diseases.
Empowering insights: We translate complex scientific data into actionable knowledge, putting you in control of your well-being.
Support Independent Journalism - Subscribe Today!
Don't miss out on valuable insights! Join our community of informed readers for free today. As a free subscriber, you will get an email granting you access to the full article within a few days. You will have access to earlier articles immediately.
Immediate access is available to paid subscribers. Your continued support means the world to us.
Keep in mind that this delay could be eliminated for free subscribers with just 115 more paid subscribers. Help us make this accessible without delay for everyone by becoming a paid subscriber today.
KP.2: New Study
Before we get into the latest study, it’s important to keep another study in mind. A pre-print study published on February 23, 2024, showed that JN.1 was able to effectively infect people that hadn’t been infected within the prior 6 months and that the immune response people had after an XBB infection, waned quickly so that by after 6 months, there was almost no protection left.
A study published on April 26, 2024, showed that KP.2 further reduces the efficacy of the XBB.1.5 booster and the immune response from a JN.1 infection. KP.2 boasts Re rates 1.22 to 1.32 times higher than JN.1 hinting at its potential to become a globally dominant variant.
As of early April 2024, the variant frequency of KP.2 had already soared to 20% in the United Kingdom and in later April it had reached 24% in the United States, underscoring its rapid spread and adaptability. However, while KP.2 displays enhanced viral fitness, the pseudovirus assay surprisingly revealed a 10.5-fold decrease in infectivity compared to JN.1. The study didn’t look at all the potential mechanisms KP.2 could employ to gain a significant advantage so the decrease they found is misleading. The fact that it is becoming dominant shows that it clearly has an advantage over JN.1.
Further investigation through neutralization assays unveiled that KP.2 exhibits significant resistance to monovalent XBB.1.5 vaccine sera, both in vaccinated individuals and those with breakthrough infections. The 50% neutralization titer (NT50) against KP.2 consistently lagged behind that of JN.1, highlighting its ability to evade immune responses.
These findings suggest a nuanced interplay between KP.2's increased immune resistance and its heightened rate of transmission. The rate of evolution is gaining momentum. We not only have KP.2, we have KP.2.2, KP.2.3, KP.3, KP.4.1, KP.4.2, LA.1, LA.2, LB.1, and more on the way.
COVID Symptoms:
Sore Throat
Cough
Runny Nose
Sneezing
Fatigue
Nasal Congestion
Diahreea
Headache
Muscle aches
Fever: Keep in mind that on average, only 17% of people have a fever. (1)
The percentage with a fever reduced with the Omicron BA.1 and BA.2 to just 14% of people. Only around 40% of people with RSV had a fever. Under 60% of people with rhinovirus or seasonal coronaviruses had fevers. This discrepancy challenges the validity of using fever as a determinant of infectiousness.
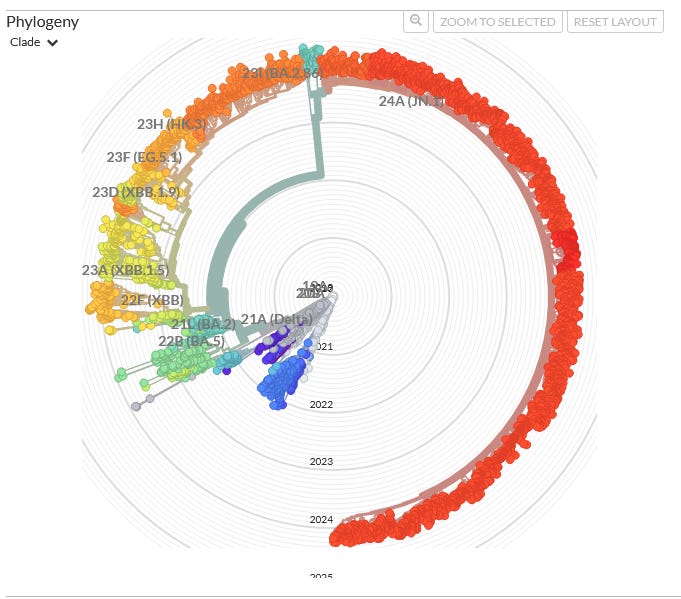
Lifting Mitigation Protections, Fueling Evolution
The graphic below shows how each year brings a broader spectrum of viral mutations and new variants. It doesn’t take much imagination to see what 2025 will look like without any change in our actions. The importance of mitigation efforts can not be stressed enough. We have to put this virus in check and prevent the emergence of even more concerning variants. The evolution of COVID is headed in an increasingly dangerous direction, becoming more immune evasive and suppressive, allowing for increasing odds of viral persistence and Long COVID.
Global-View
The W.H.O. is burying SARS-COV-2 into the May 1, 2024, Influenza Report. They report that “SARS-CoV-2 activity, as reported from sentinel surveillance in 68 countries/areas/territories that met inclusion criteria*, overall remains low. Activity is elevated and increasing in some countries in Western Africa, Western Asia, and South Asia.” The W.H.O.'s "sentinel surveillance" encompasses 68 countries, indicating that it excludes 127 countries from its coverage. The world must do better than this.
It's deeply concerning and unacceptable that the U.S. is not contributing data to the W.H.O. Why is this failure happening, and what needs to be done to address it?
Sequence Count by Country
Alarm bells are ringing. Only 33 countries are currently reporting sequencing data on the virus. While the U.S., Canada, the U.K., Australia, China, and Japan contribute significantly, this leaves a massive blind spot. With 162 countries lacking representation, we're flying blind. We urgently need a global push to expand sequencing efforts. This critical data is essential to understanding the virus's evolution and warning people about what to expect.
The Variant Watch List
JN.1.11.1, LA.1, LA.2, JN.1.7.4, KP.1.1.1, KP.2, KP.2.2, KP.2.3, KP.3, KP.4.1, KP.4.2 JN.1.4.4, and LB.1
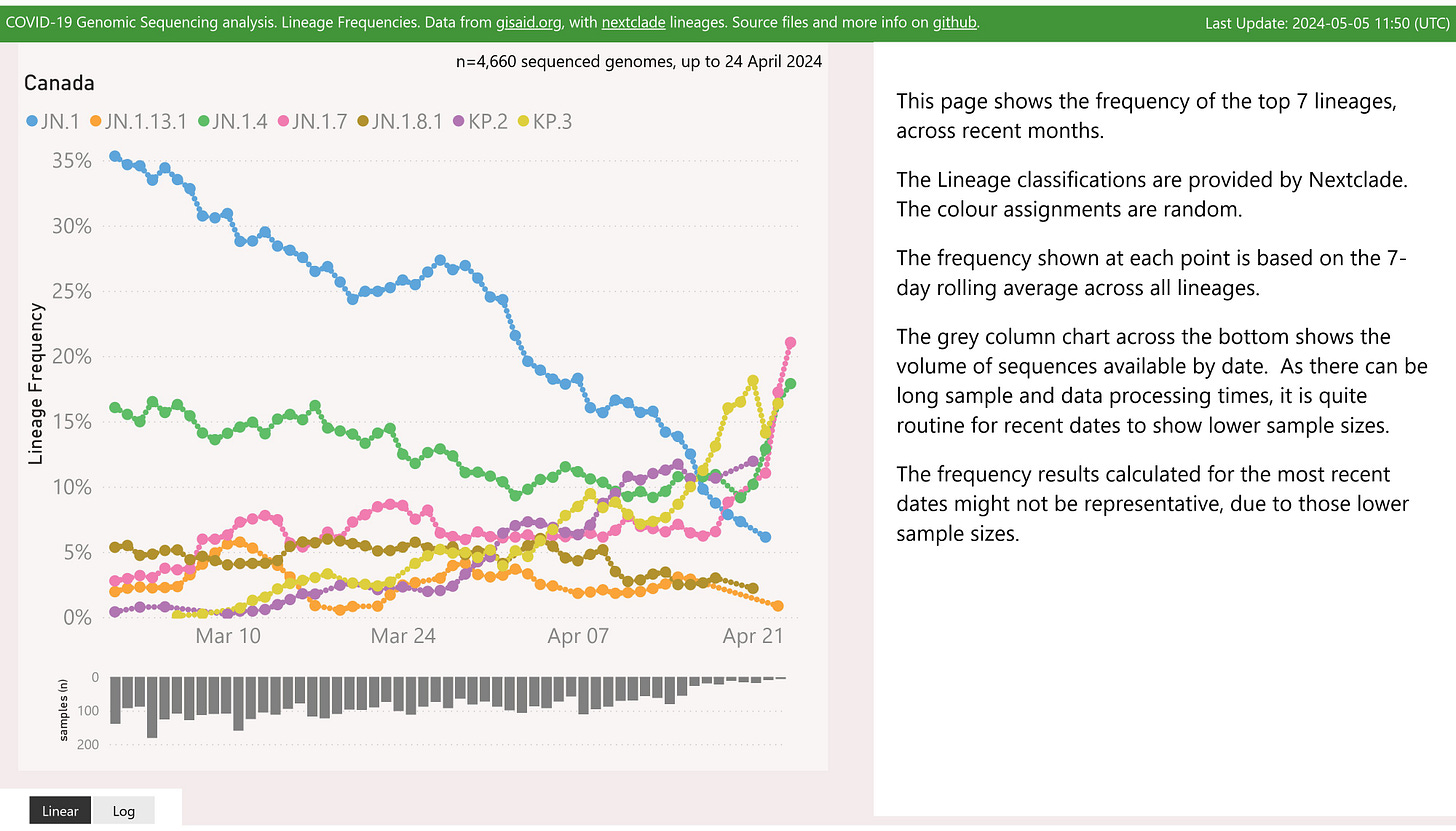
Canada
Note that JN.1.4, JN.1.7, KP.2 and KP.3 are all increasing in prevalence, with JN.1.7 appearing to have the highest rate of growth. JN.1.7.2 and/or JN.1.7.4 may be behind the increase, but KP.2 and/or KP.3 will still likely take the lead unless a new mutation or two are acquired by any of these variants.
SARS-CoV-2 Strategies for Innate Immunity Evasion
This section is from the March 16, 2024 update. It’s important so if you didn’t see it, here it is again.
Blocking Interferon Production & Response:
Interferons (IFNs) are crucial signaling proteins that coordinate antiviral responses. SARS-CoV-2 employs multiple proteins (e.g., NSP1, NSP3, ORF6, N) to impede IFN production and disrupt their signaling pathways. This prevents early viral clearance and blunts the body's rapid response.
Targeting Key Antiviral Pathways: Innate immune cells use sensors to detect viruses and trigger responses. SARS-CoV-2 proteins (like Nsp15) can directly interfere with these sensors and suppress the crucial antiviral pathways they activate.
Manipulating Host Cell Processes: The virus hijacks host cell machinery to support its replication. Some studies suggest SARS-CoV-2 manipulates cellular stress responses, autophagy (a recycling process), and pathways relating to inflammation. This disrupts the cell's ability to mount an effective innate immune response.
Sources:
Innate immune evasion strategies of SARS-CoV-2 | Nature Reviews Microbiology: [https://www.nature.com/articles/s41579-022-00839-1]
Insight into the mechanisms of coronaviruses evading host innate immunity - NCBI: [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9968664/]
The molecular mechanism of SARS-CoV-2 evading host antiviral innate immunity - Virology Journal: [https://virologyj.biomedcentral.com/articles/10.1186/s12985-022-01783-5]
TACT’s Overview:
The KP variants and others like them will very likely cause people to have varying degrees of symptomatic infections. If you haven’t been infected or vaccinated in over 6 months, it’s likely that you don’t have any immunity to these variants. Even if you still have an immune response to the older variant, it is still likely to infect you.
For many, if not most people, especially if not exposed to a high viral load, they will quickly build a strong spike-specific T-cell response, which can quickly eliminate COVID-infected cells. (2) These will likely be shorter asymptomatic infections or mildly symptomatic. Anytime a virus evades antibodies and requires T-cells, we are losing cells and new cells have to divide to replace the lost cells, so even in this best-case scenario, COVID is accelerating aging at the cellular level. (3)
For people exposed to higher viral loads or who have weaker immune systems, the virus will be able to replicate, circulate, and potentially infiltrate into the viral reservoirs where it can persist. In many of these cases, people may still have no symptoms or mild symptoms, because the virus is so effective at evading and infecting cells of the immune system. The lack of an immediate, strong immune response doesn't necessarily equal safety – the damage may be happening silently. Sadly, in many cases, there are long-term health implications of COVID without any symptoms.
Without having low-cost, effective tests, and many not having symptoms, it is nearly impossible to determine which category you will fall into until it is too late. For those of us who have symptoms, even if mild, do not dismiss them because for Paxlovid to have the best chance of working, it has to be started as soon as possible. Metformin has shown to be the better option at this point, but it has yet to be approved for COVID-19. In either case or if taking both, starting early is key for the best outcomes.
COVID Summer Forecast
COVID prevalence baseline is still unacceptably high, despite being at the lowest point it will likely hit for the rest of the year. We can expect overall prevalence to remain flat with some local variations. Even in the face of these variants, the prevalence is unlikely to increase because schools are ending for summer break. If you are in a country with schools that will be in session for a number of weeks, like Australia, then it is likely they will spread through schools, leading to exponential growth, and thus wastewater prevalence will increase. In the U.S., it will likely begin increasing by mid-June, possibly a little earlier, particularly in the Southern states. The prevalence will start increasing at a faster pace into July and August, and peak in the first couple weeks of September. The peak is likely to go quite a bit higher than last summer.
In short, this summer is unlikely to be as smooth as last summer, when nearly everyone had a strong immune response to the XBB variants. We have highly mutated, immune escape variants, and a quickly waning immunity from those infected in November, December, and January. These variants can evade that immunity but if less than 6 months from that infection, it may help provide nominal protection.
The speed at which new variants are popping up and the direction of evolution is extremely concerning. KP.2 has a higher immune escape than JN.1 and all the variants before it. The KP variants and their offspring are increasing the odds of persistent infections, which lead to immune dysregulation, autoimmune diseases, brain damage, nervous system dysfunction, and other cascading issues including serious mental health challenges. The toll this takes on families is huge. The increasing stress on businesses and the economy is growing.
We urge individuals to actively advocate for their local, state, and national leaders to take decisive action. This entails securing funding and enacting legislation that prioritizes air filtration and ventilation to effectively combat airborne transmission in schools and hospitals. It's imperative to demand that public health guidance aligns with scientific evidence, free from the influence of political figures beholden to billionaires or corporate interests.








Thanks for continuing to write about the covid pandemic. So many important voices have ceased to inform the public and I fear that H5N1 is accelerating this process.
Unfortunately, this statement
"For many, if not most people, especially if not exposed to a high viral load, they will quickly build a strong spike-specific T-cell response, which can quickly eliminate COVID-infected cells. (2)"
is not necessarily true. 'quickly eliminate' might not be the best term to use. 'quickly control' (perhaps?) This virus is very persistent. In the reference below, these researchers used a sophisticated technique to look for T-cell activation up to 2.5 years post Covid-19. From the reference...
"We identified cellular SARS-CoV-2 RNA in rectosigmoid lamina propria tissue in ALL these participants, ranging from 158 to 676 days following initial COVID-19 illness, suggesting that tissue viral persistence..."
https://www.medrxiv.org/content/10.1101/2023.07.27.23293177v1