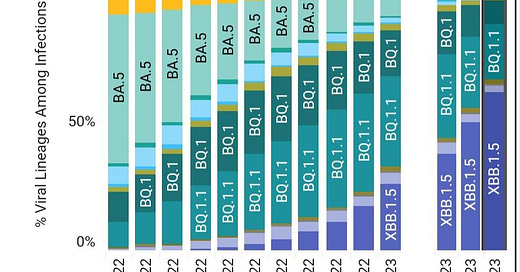
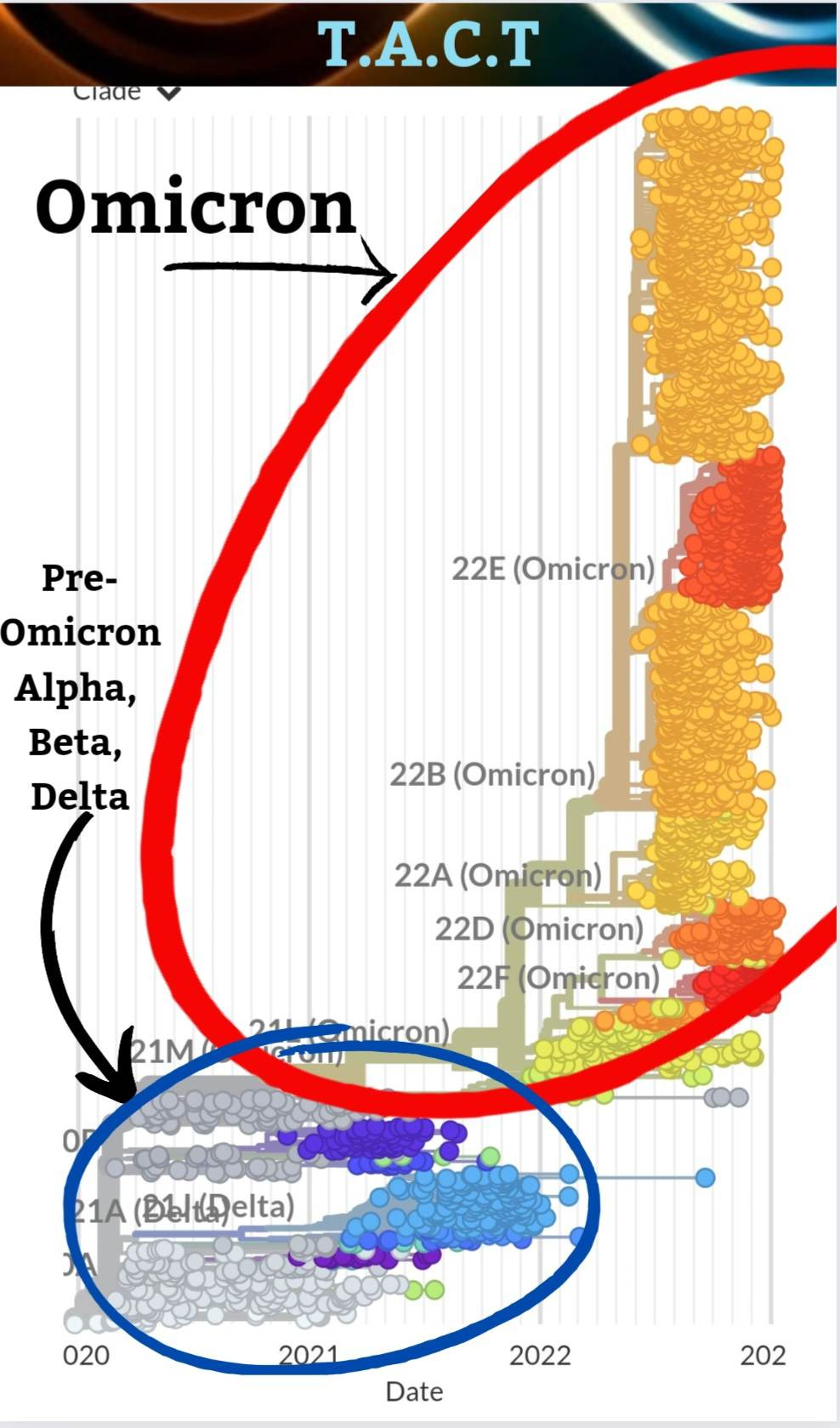
XBB.1.5 increases to over 60% of sequenced cases.
What might XBB.1.9 do to make it harder for our immune system to fight?
XBB.1.5 makes up over 60% of sequenced cases in the U.S., according to the CDC. This variant continues to expand across North America. This is the most antibody-evading variant to date, which means anyone can become infected.
XBB.1.5 seems to spread faster in areas that have more vaccinated people, but anyone can get it, and it can infect organs, including the brain. This is so important to understand because it doesn’t matter if you have been vaccinated or have never been vaccinated; everyone is susceptible.
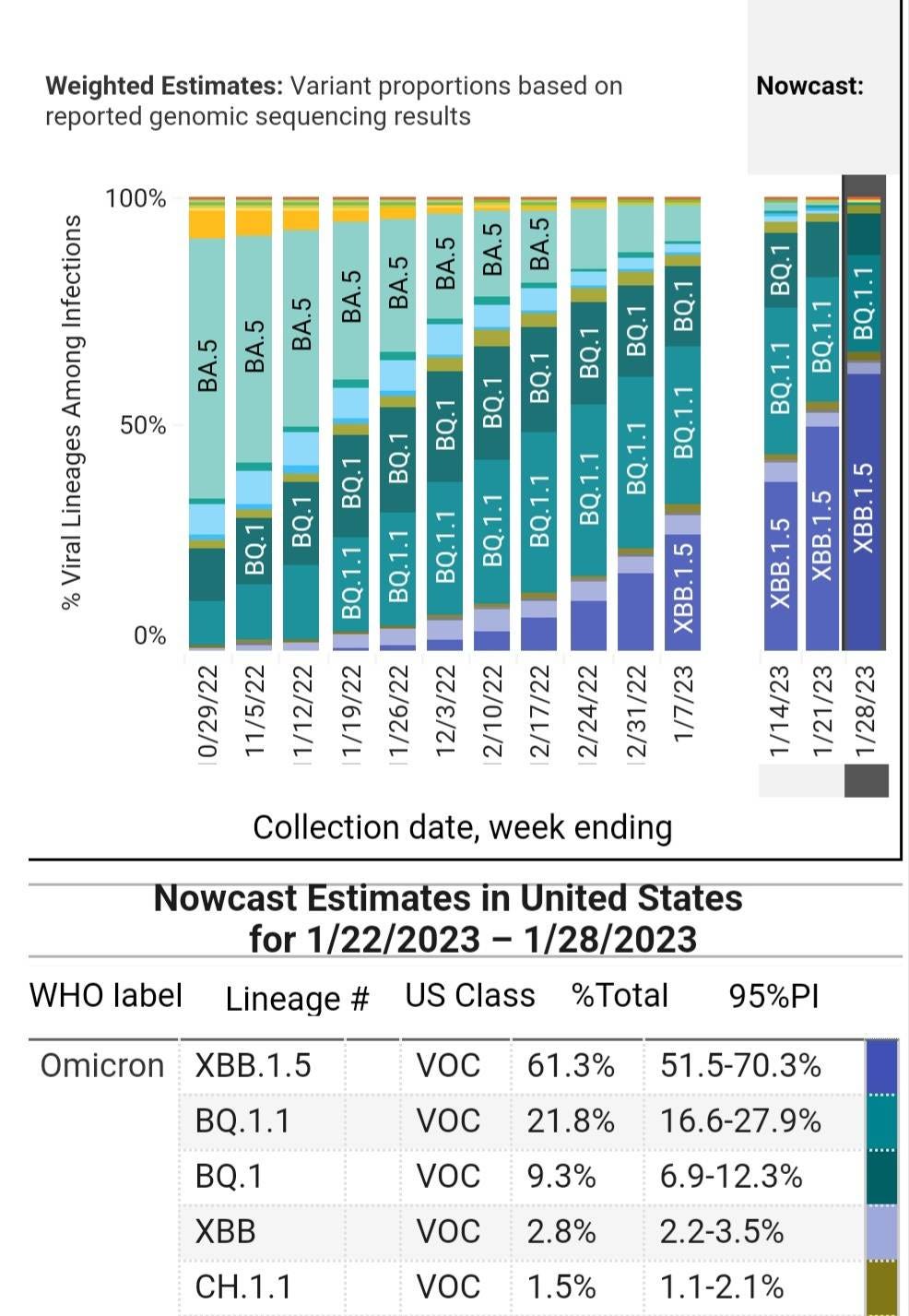
Without any action to prevent transmission, people are exposed to more respiratory droplets filled with viral particles when near an infected person. The more someone is initially exposed to, the more likely it is that it will weaken the immune system and infect organs. According to Walgreens COVID data, people who have recently been boosted have slightly lower odds of infection, followed by people who have never been vaccinated. If you have been vaccinated and it has been over 3 months since the last shot, the odds of infection are much higher.
Walgreens COVID-19 Index
The decline in the positivity rate is already leveling off, as expected. Many states, shown in shades of red, are now seeing the positivity rate increase quite a bit. As these highly contagious variants are spreading again between schools and homes, this trend is likely to continue.
As noted previously, in New York, the XBB.1.5 is declining while new variants are now taking over. The question is, if XBB.1.5 is so good at avoiding antibodies, what can the next generation of variants do to make it even harder for our immune system to fight it?
XBB.1.9.1 Child of recombinant of BJ.1, BM.1.1.1
196% growth advantage (early estimate so will likely change)
Prominent mutations
ORF1b:V1092F
N:T362I
Without doing a deep dive into this variant, the N:T362I mutation jumps out because it is yet another mutation in the N-protein, not the S-protein. These mutations impact T-cells, our last line of defense.
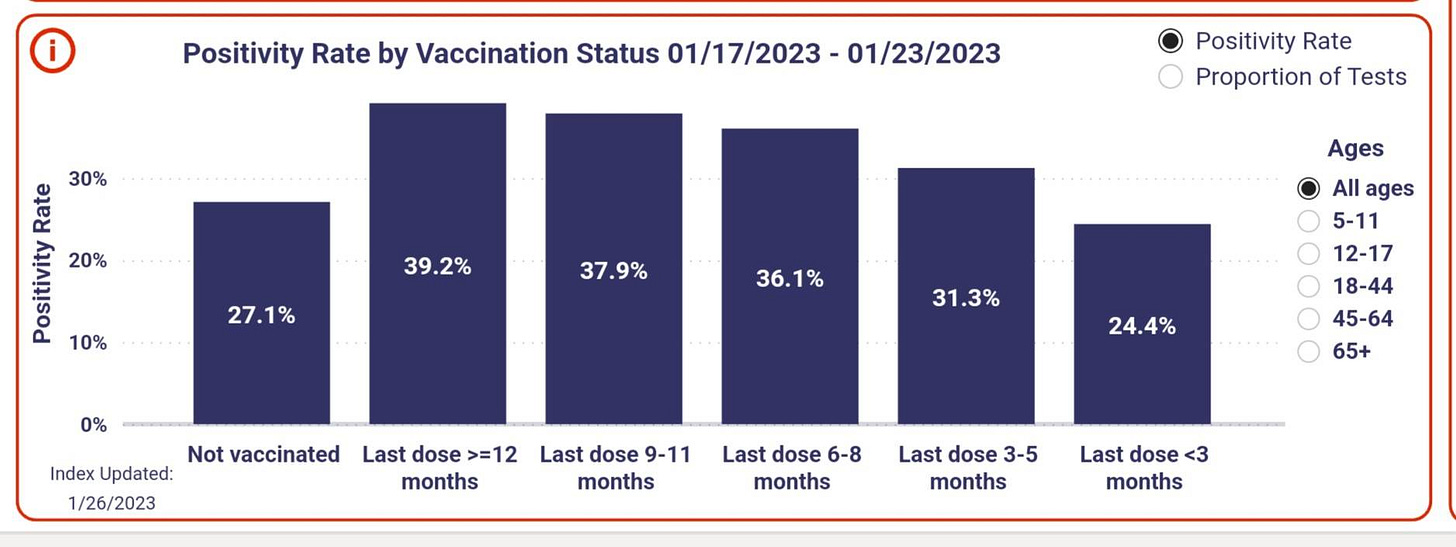
XBB.1.9.1 has seed cases all over the world and is increasing the most in the countries above. Five cases have already been sequenced in the U.S.
“The SAR-CoV-2 N-protein plays pivotal roles in inflammation, cell death, innate antiviral immunity, and adapted antiviral immunity.” (1)
How could changes in the N protein give COVID an advantage?
The XBB variants crushed the antibody response, so what is the next best way for COVID to gain an advantage? If it were to gain an advantage above that of XBB.1.5 by a mutation in the N-protein, then the most likely answer is to beat the next most common immune response. That is the T-cell response. Selective pressure tends to dictate COVID’s evolution.
“The adaptive cellular immune responses rely on both CD4+ T cells to secrete cytokines for the functional support of CD8+ T cells and B cells, and on CD8+ T cells to eliminate the virus by killing infected cells.” (4)
“These results, particularly the different reactivity of NT362I and NT362K, implied that the charge of the amino acid side chain, at least, might influence the binding affinity of N361-369 to HLA∗A11:01*. We also found that the N361-369 homologous peptide from MERS-CoV (NMERS), which exhibited 3 amino acids in difference to N361-369, bound to HLA∗A11:01 weakly" "Interestingly, the TCR 4-T cells were mainly activated by N:T362I or N:F363L"(4)
If the N:T362I mutation activates CD4 T-cells, then that could increase viral replication while interrupting the job of the CD4 T cells in helping the CD8 T cells. At least one study has shown this is already happening. "Once inside T helper cells, SARS-CoV-2 assembles viral factories, impairs cell function, and may cause cell death.” “SARS-CoV-2 infected T helper cells express higher amounts of IL-10, which is associated with viral persistence and disease severity. Thus, CD4-mediated SARS-CoV-2 infection of T helper cells may explain the poor adaptive immune response of many COVID-19 patients." (9)
If the mutation prevents cytokines from being released, the immune response could be less effective. If it causes more cytokines to be released, there could be more inflammation and problems with blood vessels, leading to vascular dysfunction. Any changes that weaken or alter the T-cell responses could have serious implications. The evolution of the virus is headed in a very dangerous direction. We know that this virus has the capacity to become more dangerous. The data is starting to point in that direction. The more widespread transmission there is, the faster the evolution. COVID is evolving at a faster pace than ever before.
What is the mechanism that escalates the MERS fatality rate from COVID?
According to the WHO, approximately 35% of patients with MERS-CoV have died” (5) Another study shows the case fatality rate at 32.7%. (6) If there is any chance that evolution is moving towards something closer to how MERS impacted people, then we should all be working towards limiting transmission.
Are we headed in that direction? Hopefully, it will never become anything like MERS, but wait, it is already similar to MERS.
“MERS-CoV efficiently infected T cells from the peripheral blood and from human lymphoid organs, including the spleen and the tonsil."(14) COVID also infects T-cells and persists in the tonsils.
“Asymptomatic yet persistent infection in children's tonsils suggests that lymphoid tissue may play an important role in community transmission.” (15)
➡️ “CD123+dendritic cells were the most infected cells, followed by CD14+ monocytes, CD4 & CD8 T-cells.” (15) MERS-CoV could infect dendritic cells. (14)
Is COVID evolving to further limit or suppress the last layer of our immune defense, the T-cell response?
”SARS-CoV-2 N-protein induces stronger CD8+ T cell responses in COVID-19-recovered individuals.” “Furthermore, the corresponding CD8+ T cells can be maintained for months with preserved antiviral efficacy to various SARS-CoV-2 strains” (1)
Most people who have been infected have a strong CD8+ T cell response to COVID because of the N-protein target. This would be good if the virus wasn’t evolving to get better at avoiding or attacking our immune system. We already know that a certain percentage of T-cells become infected and die when infected with COVID, so this isn’t a far fetched idea. This is already occurring. “This work confirmed a SARS-CoV-2 infection of T cells, in a spike-ACE2-independent manner, which shed novel insights into the underlying mechanisms of SARS-CoV-2-induced lymphopenia in COVID." (10)
The T and B cell loss is already so bad in many people that COVID is listed next to AIDS as the leading causes of lymphocytopenia. "People with lymphocytopenia experience recurrent infections or develop infections with unusual organisms, which is a risk factor for the development of cancer and autoimmune disorders." (11)
COVID infects neutrophils, another important part of the immune system. “Neutrophils make up the largest number of white blood cells. They kill and digest bacteria and fungi to help your body fight infections and heal wounds." (16)
“SARS-CoV-2 Dysregulates Neutrophil Degranulation and Reduces Lymphocyte Counts.” "Infected neutrophils had a direct effect on peripheral blood lymphocyte counts, with decreasing numbers of CD19+ B cells, CD8+ T cells, and CD4+ T cells." (17)
“Lymphocytopenia in COVID-19 is accompanied by B cell depletion in hematopoietic tissue, which might impede the durability of the humoral immune response to SARS-CoV-2" (12)
This study shows that immune system problems can last for at least 8 months after a mild to moderate COVID infection. That is when the study ended.
"Both HIV and SARS-CoV-2 induce major changes in the lymphocyte count... “The total absolute numbers of T cells and, in particular, the CD8+ subpopulation, are lower in COVID-19 patients compared to AIDS, while the CD4+ are reduced in both at similar levels." (13)
It is clear that COVID is already suppressing the immune system, infecting organs and persisting for months, years, and likely for life. Evolution is moving towards more efficient immune suppression and dysfunction. Changes to impact the T-cell response could cause COVID to become more severe and deadly. We do not have any new vaccines lined up and treatments are losing efficacy.
Strategies to Avoid COVID and Other Respiratory Viruses
We must do better to provide a safe learning environment.
Flu, RSV, and COVID are Preventable
We have the technology, we simply must utilize it.
Click the picture below to find out more and support the campaign
to provide Clear Air for Kids.
Note: We appreciate you sharing our content with others and leaving your thoughts in the comments.
Definitions:
* HLA-A11 (A11) is a human leukocyte antigen serotype within the HLA-A "A" serotype group. The serotype is determined by the antibody recognition of α11 subset of HLA-A α-chains. For A11, the alpha "A" chain is encoded by the HLA-A*11 allele group and the β-chain is encoded by B2M locus.” (3)
**Binding dimerization “Dimerization plays a critical role in the regulation of another family of transmembrane proteins, the receptor tyrosine kinases. Specifically, ligand binding to the extracellular domain allows the intracellular kinase domain to dimerize and cross-phosphorylate at regulatory sites, leading to activation of the intracellular kinase domain." (8)