W.H.O. Recognizes Airborne Transmission/ In-Depth Analysis: The W.H.O.'s Tool for Evaluating Airborne Transmission Risk in COVID-19
A Step-by-Step Guide and Future Implications
The recent release of an official document by the World Health Organization (WHO) acknowledging airborne transmission marks a significant milestone. Although some WHO officials had previously acknowledged the airborne nature of SARS-CoV-2 in public statements, this aspect had been omitted from official documents until now. Backed by science and data, this acknowledgment represents a crucial step forward.
Today, we're delving into the WHO's online tool, ARIA (Airborne Risk Indoor Assessment), designed to evaluate the risk of airborne transmission of COVID-19. By inputting various parameters such as temperature, humidity, SARS-CoV-2 variant, space dimensions, duration of exposure, occupancy, host immunity, and event specifics like mask usage, short-range interactions, ventilation, and air filtration, users can assess their risk level. However, despite its detailed parameters, the tool does have limitations that may not be immediately apparent upon first use.
We'll take you on a guided tour through this tool, unveiling its functionality screen by screen, and pointing out how to navigate around the flaws along the way. While our example simulates a classroom setting without ventilation or air filtration, it's important to note that the tool is not typically used for schools, thus introducing certain limitations. Nevertheless, by being able to explore various scenarios across different settings, we can gain insights into potential risks and better advocate for enhanced safety measures.
Prepare to be surprised by the realism of the simulated results, highlighting the tool's potential impact. Understanding these dangers empowers us to advocate for stronger safeguards. Feel free to follow along by clicking the link provided below, to explore the tool firsthand. Let's embark on this journey together.
ARIA (Airborne Risk Indoor Assessment) Tool
https://partnersplatform.who.int/tools/aria/calculator
Note: Some of the comments on each slide below and in totality may be subjective, so use your discretion.
The first question inquires about adding a location, which may not necessarily contribute to the main purpose of using this tool. Whether to include a location is at your discretion. Additionally, it seems that many cities in the U.S. are not listed as options.
For this example, we are clicking, I don’t know.
Do you know the temperature and humidity level in the space?
We can assume most spaces will be around 70 degrees Fahrenheit or 21.1 degrees Celsius. The humidity may change significantly without proper ventilation, and it’s hard to know what the humidity will be at the time of the event. Humidity is generally between 30% and 50%. For this example, we are putting 50%.
Do you know which is the dominant SARS-CoV-2 variant in your area?
Without localized sequencing, and very little, if any, in many places, the in-your-area part is unlikely to be known. If we did know, the type of variant stops at Omicron. We know that COVID has evolved incredibly far since the first Omicron variant. Without being able to designate a particular variant through a pango lineage designation, like JN.1, or KP.2, the point of asking this question is pointless. Everyone will answer, “Omicron”
How big is the space?
The room dimensions are in meters so we have to do some calculations if converting to feet. 1 meter = 3.28 feet 10 feet = roughly, 3 meters 30 feet = roughly, 9 meters
1000 square feet = roughly, 92 square meters
How long will the event last?
Note that the time is 24 hours so 3:00 pm, would be 15:00. The example below has since been updated.
Will the person infected with COVID-19 be present during the entire event?
We have to assume that someone will be infected for the entire event, but we don’t know how many. The fact there is an option for NO is ridiculous unless it is a risk assessment for an infected person to attend the event.
We are answering Yes in our example, but if you were to click on No, you get this additional drop-down box.
It seems like this message is aimed at someone who knows that another person is infected. In our scenario, it could be a parent who is considering whether to send their child to school for half a day to avoid being marked absent and having to provide a doctor's note. (This highlights another significant issue that needs attention.)
How many people will be there (including people infected with COVID-19)?
Number of people infected with COVID-19 attending the event (minimum 1). This number is almost always an assumption. You may start with 1, and increase the number to understand how this variable impacts the risk assessment.
A notable exception to increasing the number of infected above 1, is if you checked off Conference/Training. The example below was updated to 1 infected person.
Did the persons attending the event receive a COVID-19 vaccination more than 14 days ago?
This is another place that could mislead people. Considering that vaccination rates are so low, and we know that vaccines don’t prevent infections, we can click “NO”.
This screen notably omits school classrooms but includes universities. However, schools often have facilities such as gyms and cafeterias, which are similar to restaurants. In this example, we're selecting "conference/training" to represent a classroom. We provided the dimensions of the space at the outset.
Although it's appreciated that the question was asked, it's important to note that it doesn't specify the type of masks that will be worn. There's a significant difference between properly fitted N95 masks and surgical or cloth masks. Without specifying the type of mask, we're left to assume that this question provides minimal benefit.
Will short-range interactions (less than a 2-meter distance without masks) take place at the event? 2 meters = 6 feet 6.74 inches.
In settings ranging from classrooms to restaurants and beyond, the answer is likely to be YES.
Once we click YES, we're prompted to input various times for short-range interactions. In this scenario, we are assuming 2 hours, between 10 and 12.
Note: Start interaction time must be between start and end time. In this example, the start time was updated from what is in the pic below to 10:00 and the end time was updated to 12:00.
Will the space be mechanically ventilated?
While this question may be helpful for a building manager, it might not be relevant to the average person. In this example, we're selecting "I don't know" since we're focusing on the perspective of the average individual.
Will windows be open?
For our example, we are saying No.
Will there be air filtration devices in the space?
For our example, we are clicking on No, but you can always go back and add it to compare the difference in their results.
Then we can click, Finish
All steps completed
That takes us to this screen, where we can go back and change inputs or see the results.
Results:
Based on these conservative responses, the risk is 32% risk of infection with short-range interactions and 6.5% without short-range interactions.
The projected number of new cases is 9.37. While the model technically doesn't specify a classroom, considering the inputs we provided, it's concerning that 9 people could potentially be infected within a single day. Although this outcome is anticipated, it's unexpected to see such results displayed by the WHO tool.
We have to keep in mind that the tool doesn't factor in the proximity to an infected person or the level of infectiousness of that person. It appears to imply that exposure won't necessarily result in infection. While it might account for individuals with a robust immune response post-infection or vaccination, it lacks the option to address the risk of reinfection from a different variant. For instance, it doesn't consider the likelihood of reinfection from an antigenically distinct variant, such as when the JN.1 variant quickly replaced the XBB descendant variants.
A significant aspect of this tool and its associated paper is the acknowledgment by the WHO of airborne transmission, which is likely to influence how the CDC and other public health agencies revise their future guidance. This could initiate a chain of events, potentially leading to updates in OSHA standards and building code requirements. It marks an important milestone, hopefully paving the way for enhanced protections and improved health outcomes in the future.
The W.H.O. lists the following limitations that must be considered.
Limitations: The Tool is not meant to replace a comprehensive risk assessment.
The Tool is subject to inherent limitations and assumptions, which are important to acknowledge for a comprehensive understanding of the Tool’s scope and accuracy.
Complexity of Transmission Dynamics: The aerobiology of infectious particles and the transmission dynamics of viruses in humans are intricate and multifaceted. Various factors, including particle size distribution, environmental conditions, indoor air flows, and virus characteristics, can significantly impact the transmission process.
Variability in Data: The model relies on available scientific data and literature. However, there may be limitations in the quality and quantity of data for some variables, leading to potential biases and uncertainties in the results.
Parameter Values: The accuracy of the model depends on parameter values used for calculations. Despite efforts to extract and update these values, they are subject to ongoing research and may change over time, affecting the model's reliability.
Long-Range Transmission Assumption: The model assumes a well-mixed approach for long-range transmission, which may not fully represent real-world scenarios. Fluid dynamics simulations, while more precise, pose practical challenges in terms of computational capacity and expertise.
Short-Range Transmission: Short-range transmission may be influenced by other factors such as posture and airflow interactions, introducing additional complexity and uncertainty.
Host-Pathogen Interaction: Variables related to host-pathogen interaction, including viral load, dose-response, and host immunity, are influenced by multiple factors, making accurate estimation challenging. The model employs a probabilistic approach and the precautionary principle to address these limitations.
Post-Infection Immunity: The model currently considers only vaccine-induced immunity due to data limitations. Other post-infection immunity is not included for now, potentially leading to an underestimation of risk.
Number of Infectors: The model allows for calculations that consider multiple infectors, and the user must input the number of infected individuals attending an event, which requires an assumption on the part of the user.”
”Please be aware that this web application's results are presented as total probabilities, and the accuracy depends on the quality of data and statistical distributions. Regular updates may be necessary to account for evolving knowledge and data availability.”
”The use of this Tool should be accompanied by a critical understanding of these limitations, and it is advisable to consult with healthcare professionals and experts for a comprehensive assessment of SARS-CoV-2 transmission risk in specific contexts. This tool should not replace professional medical advice or public health guidelines.”
W.H.O.'s ARIA (Airborne Risk Indoor Assessment) tool
https://partnersplatform.who.int/tools/aria/calculator
The following are excerpts from the W.H.O. paper on airborne transmission risk.
“Indoor airborne risk assessment in the context of SARS-CoV-2: description of airborne transmission mechanism and method to develop a new standardized model for risk assessment”
“Description of airborne transmission mechanism and method to develop a new standardized model for risk assessment.”
“This manual leverages on both longstanding and new evidence based on the expertise of scientists from a wide variety of disciplines. It provides a new, standardized, and validated model for quantifying the risk of airborne transmission of SARS-CoV-2 in indoor settings. Our aim was to provide a robust tool to inform mitigation measures for business owners, households, healthcare centres and others, to not only reduce the unacceptable and unnecessary health burden resulting from the airborne transmission of respiratory pathogens, like SARS-CoV-2, and enable a more agile and effective response.”
“This manual aims to define a new model, with a standard method to quantify the risk of SARS-CoV-2 airborne transmission in indoor settings according to the current evidence available at the time of this publication. The model aims to inform the development of risk-based ventilation recommendations to mitigate the inhalation risk, as well as to provide an agreed foundation for future guidance related to other respiratory and potentially airborne diseases. In particular, this document aims to:
1. Define a standardized model, to quantify SARS- CoV-2 airborne risk transmission in different indoor settings including residential, public and health care settings
2. Guide the development of an online, user-friendly tool to enable the general public and building managers to assess SARS-CoV-2 airborne risk transmission in residential, public and health care settings and inform risk reduction measures.
“The new model will also provide a baseline from which to test the transmission capacity for SARS-CoV-2 variants of concern as well as other airborne pathogens and provide an agreed foundation for future guidance related to other respiratory and potentially airborne diseases.”
IMPORTANT NOTE
“While SARS-CoV-2 can spread through multiple routes of transmission, this model is only considering short- and long-range airborne transmission with short-range limited to particle inhalation and not direct deposition.”
“While this document provides guidance to Member States and regulatory bodies for the development of risk-based ventilation rates and inform future interventions, the online web application is meant to provide an accessible tool to estimate the infection risk probability in various indoor settings. General public and building managers can use this online, user-friendly tool to assess SARS-CoV-2 airborne risk transmission to inform risk reduction measures such as increasing ventilation, reducing occupancy, and wearing a higher filtration efficiency mask. Its application by Infection Prevention and Control specialists, building managers, health care facility managers and the general public will inform risk reduction measures as well as to enable informed decisions by the users.”
Glossary:
Airborne: Anything that is suspended or carried through the air [2].
Airborne transmission*: The process whereby aerosolized infectious respiratory particles (IRPs) are inhaled and enter the respiratory tract of a susceptible person, move through the upper and then lower parts of the respiratory tract, and can be deposited on the tissue at any point along the tract, but preferred sites of entry may be pathogen-specific. This mode of transmission can occur when IRPs have traveled either a short or a long distance (range) after emission from an infected person or after resuspension of deposited particles from the surface. Can also be used interchangeably with inhalation transmission.
Clean air delivery rate (CADR): The result of the measured flow rate, delivered by an air cleaning device, at which all particles of a given size distribution are removed in a given timeframe. Usually expressed as m3/h [5]
Infectious aerosol: A collection of infectious particles suspended in air, i.e., aerosolized infectious respiratory particles [15]. Infectious Respiratory Particles (IRPs)*: Particles composed of water and other constituents (including salt, proteins, mucus, etc.), containing viable pathogens exhaled in a wide range of sizes by people infected with a respiratory pathogen. Long-range airborne transmission*: Transmission occurring via inhalation of aerosolized infectious respiratory particles by a susceptible host at a distance farther than conversational distance (2 meters) from the infected person/ source of infection [16].
Short-range airborne transmission*: Transmission occurs via inhalation of aerosolized infectious respiratory particles inhaled by a susceptible host at a distance up to conversational distance (2 meters) from the infected person/ source of infection.
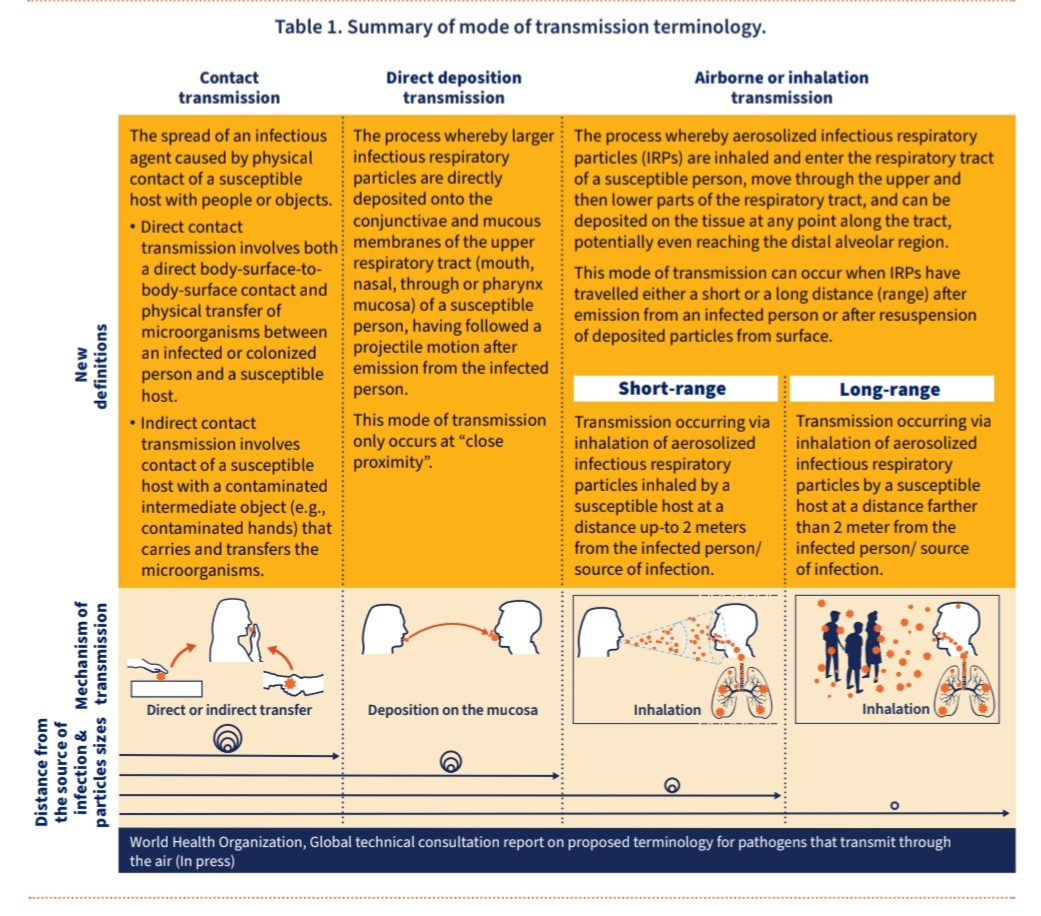
Modes of transmission
The mechanisms of infection transmission are complex, with the risk of disease determined by numerous factors that have considerable and uncertain variability, including the characteristics of the pathogen concerned, the infectiousness of the host, the media in which it passes from the source to new hosts and the immune response of the exposed host [32]–[34]. Transmission through the air complicates this further by adding other influencing factors [35] such as the dispersion and distribution of infectious respiratory particles (IRPs); the effect of temperature, relative humidity, and ultraviolet radiation on the survival of the pathogen [15], [28], amongst other factors. Respiratory viruses can spread via three major modes of transmission (Table 1).
“Airborne or Inhalation transmission*: The process whereby aerosolized infectious respiratory particles (IRPs) are inhaled and enter the respiratory tract of a susceptible person, move through the upper and then lower parts of the respiratory tract, and can be deposited on the tissue at any point along the tract, potentially even reaching the distal alveolar region. This mode of transmission can occur when IRPs have traveled either a short or a long distance (range) after emission from an infected person or after resuspension of deposited particles from the surface. See also Figure 1. Direct deposition transmission*: The process whereby larger infectious respiratory particles are directly deposited onto the conjunctivae and mucous membranes of the upper respiratory tract (mouth, nasal, through or pharynx mucosa) of a susceptible person, having followed a projectile motion after emission from the infected person. This mode of transmission only occurs at a short range, or what can be described as at a “conversational distance” [1]. See also Figure 1.”
“When people are in close proximity, transmission of infectious particles can occur through direct inhalation (short-range) and deposition onto the mucous linings of the respiratory tract and ocular membranes of a susceptible host. The ‘long-range’ transmission can occur in indoor, enclosed settings when infectious particles accumulate over time in a given volume, at room scale, where the viral concentration is sufficient enough to cause infection once infectious particles are inhaled by a susceptible host. The concentration of infectious particles in the air can increase rapidly with poor ventilation, a small volume of air in an enclosed indoor space, overcrowding (especially with the presence of multiple infected individuals), and the amount of time spent in the space by the infected person [39]. Quantifying the probability of SARS-CoV-2 infection through the inhalation mechanism is essential to inform the development of risk reduction measures such as indoor risk-based ventilation standards.”
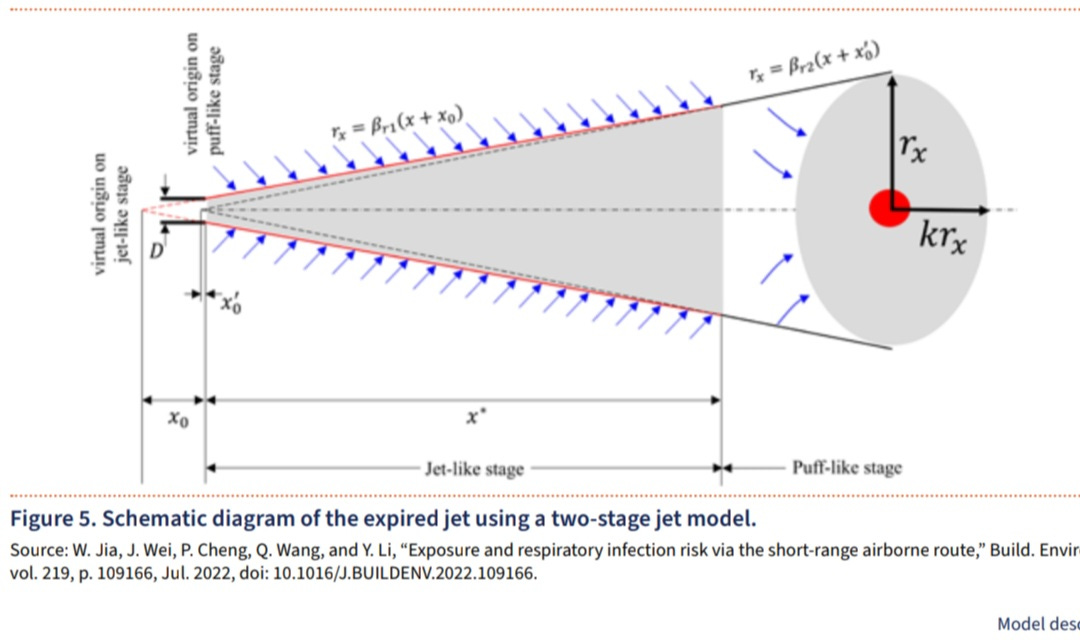
Expiratory Jet
“Besides physical distancing, indoor ventilation can significantly impact short-range airborne transmission risk [138]. This model integrates the newly developed approach to assess the infection risk via the short-range route through the two-stage jet model (Figure 5) [68]. While for long-range transmission the key parameters affecting the final virions concentration in the model are dilution by ventilation, filtration, settling and biological decay, as described above, for short-range transmission the dilution factors in the expired jet zone are governed by the buoyancy-driving flow pattern of the jet, including different mechanisms such as the exhaled flow velocity, jet-like to puff-like separation, penetration distance and indoor ventilation rate. In this regard, knowing the average initial concentration at the origin of the jet (the mouth or nose), enables the two- stage jet model to estimate the average concentration at a given distance, and an average concentration in the room zone [68]”
“This paper describes studies/outbreak investigations in indoor settings such as restaurants, public transport, workplaces, or choir venues. Long-distance airborne transmission was likely to have occurred for some or all transmission events in 16 studies and was unclear in two studies.”
“Long distance airborne transmission of SARS-CoV-2: rapid systematic review” (June 2022)
https://www.bmj.com/content/377/bmj-2021-068743
Long-range airborne was identified as the main mode of transmission, is related to superspreading events where the infector was likely to be classified as a super-emitter shedding higher than average viral loads and emitting more infectious particles.”
“Indoor airborne risk assessment in the context of SARS-CoV-2: description of airborne transmission mechanism and method to develop a new standardized model for risk assessment”
https://iris.who.int/handle/10665/376346
ARIA is an online tool that enables users and building managers to assess the risk of SARS-COV-2 (COVID-19) airborne transmission in residential, public, and healthcare settings. The aim is to inform decisions that can significantly reduce the risk of transmission.
Click Here: ARIA (Airborne Risk Assessment Tool)
Please share any questions or insights you may have.


























Thank you as always. Don’t hold your breath waiting for osha to change standards. Osha does not find any organization responsible for covid19 deaths. Businesses will lobby for no changes. Every place will say that they can’t afford to supply clean air. The usa doesn’t require access to clean water or electricity- they certainly won’t require access to clean air.
The few people wearing masks wear a surgical mask or a cloth mask. Occasionally I see someone wearing a n95.
People don’t think covid is a thing anymore. They get sick and have no idea why they are sick.🤦🏾♀️