New Study Reveals COVID-19 Can Persist in Lungs Long After PCR Tests Come Back Negative
COVID Pneumonia and Undercounting COVID Deaths
A recent study has shown that COVID-19 can persist in the lungs long after PCR tests detect the virus. This has important implications for patients who go to the hospital with persistent lung infections in the weeks and months after the initial infection. In many cases, the patient has an asymptomatic infection and never knew they had COVID. Doctors may assume that the patient is not suffering from COVID-19 after the PCR tests come back negative. However, this can not be assumed at all.
COVID-19 can persist in the lungs, tonsils, adenoids, and other places for months or even years, while PCR tests may not detect it. Looking back at the past three years of excess pneumonia deaths, we can now understand that many of these cases were actually caused by COVID-19. These findings indicate that the true impact of COVID-19 on public health may be significantly underestimated.
The study found that SARS-CoV-2 infection can persist significantly longer than suggested by standard PCR-negative tests, with specific infection of specific cell types in the lung. Despite apparent virological remission, lung pathology was similar to that observed in acute COVID-19 individuals, including micro- and macro-vascular thrombosis (67% of cases), vasculitis (24%), squamous metaplasia of the respiratory epithelium (30%), frequent cytological abnormalities and syncytia (67%), and the presence of dysmorphic features in the bronchial cartilage (44%).
The study also found that SARS-CoV-2 antigens were not detected in the respiratory epithelium, but antibodies against both spike and nucleocapsid revealed the frequent (70%) infection of bronchial cartilage chondrocytes and para-bronchial gland epithelial cells. In a few patients (19%), researchers also detected positivity in vascular pericytes and endothelial cells. Quantitative RT-PCR amplification in tissue lysates confirmed the presence of viral RNA.
These findings indicate that SARS-CoV-2 infection can persist significantly longer than suggested by standard PCR-negative tests, with specific infection of specific cell types in the lung. We have vastly undercounted the number of deaths from COVID related pneumonia. Pneumonia was listed as the primary cause of death in many cases. This is why deaths from pneumonia have remained well above the pre-pandemic average.
COVID Pneumonia
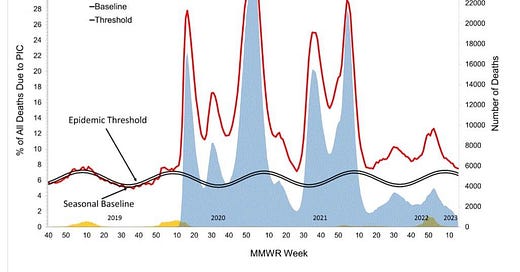
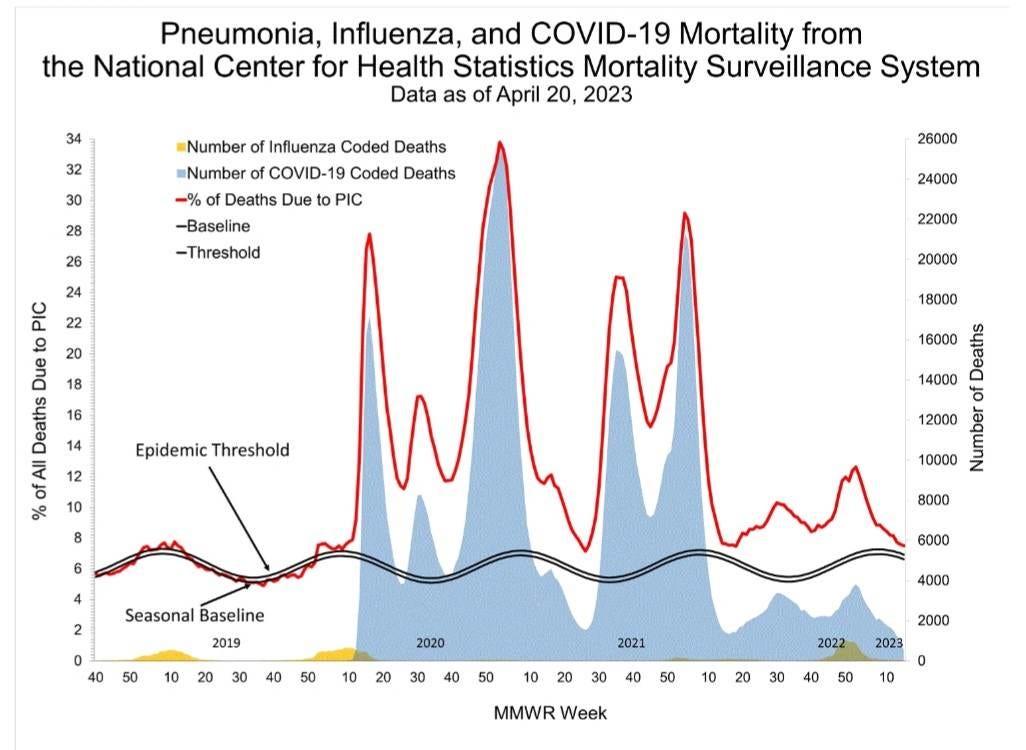
Looking at the graph below we can see that the deaths from Pneumonia, Influenza and COVID are still above the Epidemic threshold. COVID Pneumonia is very likely, not being recorded as COVID deaths in a large number of patients. Pneumonia is killing more people than COVID and Flu combined right now. The reason it isn’t recorded is because by the time people go to the hospital the PCR tests are coming back negative. They are missing the fact that COVID can persist in the tonsils, adenoids, and lungs long after the initial infection and that isn’t showing up on the PCR tests.
Pulmonary fibrosis can be a manifestation of asymptomatic or mild COVID. This study, published May 2022, said, "On evaluation, after excluding other causes, the fibrosis was attributed to asymptomatic or mild COVID illness in the past." They note that there is no definitive treatment for post-COVID fibrosis of the lungs.
This study published in November 2022, “Increase of mast cells in COVID‐19 pneumonia may contribute to pulmonary fibrosis and thrombosis”, noted a significant increase of mast cells in SARS‐CoV‐2‐infected lung tissue compared to influenza.
We see on the CDC graph above, that despite low deaths from COVID and Flu, Pneumonia is keeping the amount of deaths above the epidemic threshold. Deaths from pneumonia, flu, and COVID are still above the pre pandemic baseline and will very likely start increasing again with the latest variants and the removal of masks in hospitals. Removing universal mask use will ensure that more people suffer and die. COVID is likely leading to many more pneumonia deaths than are actually being acknowledged.
This suggests that we need to rethink our assumptions about COVID-19 and its impact on public health. We need to consider the possibility that many deaths attributed to other causes may have actually been caused by COVID-19.
In conclusion, these studies highlight the need for continued research into the long-term effects of COVID-19 and the need for more accurate testing and tracking of the virus. It also highlights the importance of taking precautions to prevent the spread of the virus, such as wearing quality N-95 masks, social distancing, opening windows, using air purifiers and all the other mitigation strategies. The true impact of COVID-19 on public health may be much greater than we previously thought, and we need to take this into account as we move forward.
The media and public health officials would have us believe that COVID has become less dangerous and is no longer a major concern. The media coverage has nearly vanished. Independent sources that are not beholden to large donors, political parties, or any other group are more important than ever. Consider becoming a paid subscriber or donating a subscription to help support this work. Thank you for your support.
T.A.C.T. is a publication supported by its readers. Consider becoming a free or paid subscriber if you are not already a member of the T.A.C.T. community.
Please let us know what you are seeing or if you have any other insights or questions.
Additional References with links:
1.2020, The burden of pulmonary fibrosis after COVID recovery could be substantial.
Progressive, fibrotic irreversible interstitial lung disease, which is characterised by declining lung function, increasing extent of fibrosis on CT, worsening symptoms and quality of life, and early mortality.
https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30222-8/fulltext
2. 2021- Lung fibrosis: an undervalued finding in COVID-19 pathological series
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30582-X/fulltext?amp=1
3. Viral Infection, Pulmonary Fibrosis, & Long COVID
interstitial changes resembled those associated with fibrotic interstitial lung abnormalities (ILA)
COVID-19 and lung fibrosis suggest that SARS-CoV-2 infection can lead to progressive lung disease
https://www.atsjournals.org/doi/full/10.1164/rccm.202211-2121ED
4.A silent march-Post covid fibrosis in asymptomatics – A cause for concern?




New technology could help detect COVID.
"Our model achieves an accuracy of 92.11% and an F1-score of 92.59% for detection of COVID-19 from CT scans."
https://dl.acm.org/doi/abs/10.1145/3551647
My wealthy sister in law said that “covid had fallen off the radar for them”…and in the same conversation she said that 3 of their best friends who are all in their early 60’s are dying from brain or pancreatic cancer…🤦🏾♀️