H5N1 Alert: New Human Case in Michigan, Dallas Influenza A Spike, Wastewater Testing Insights, and Airborne Transmission Confirmed
Highlights
Second human H5N1 bird flu infection confirmed in Michigan farmworker.
Swabbing the eyes of farm workers with eye infections confirms H5N1, not nasal swabs.
No live, infectious virus was detected in retail dairy product samples, but it was confirmed in raw milk
Need for further studies on viral particles in milk and beef products
Wastewater testing for bird flu virus to expand nationally
Heightened pandemic potential of H5N1 based on confirming airborne transmission
In a concerning development, a second human case of H5N1 bird flu has been confirmed in Michigan. This new infection has sparked renewed attention on the virus's spread and potential impact on public health.
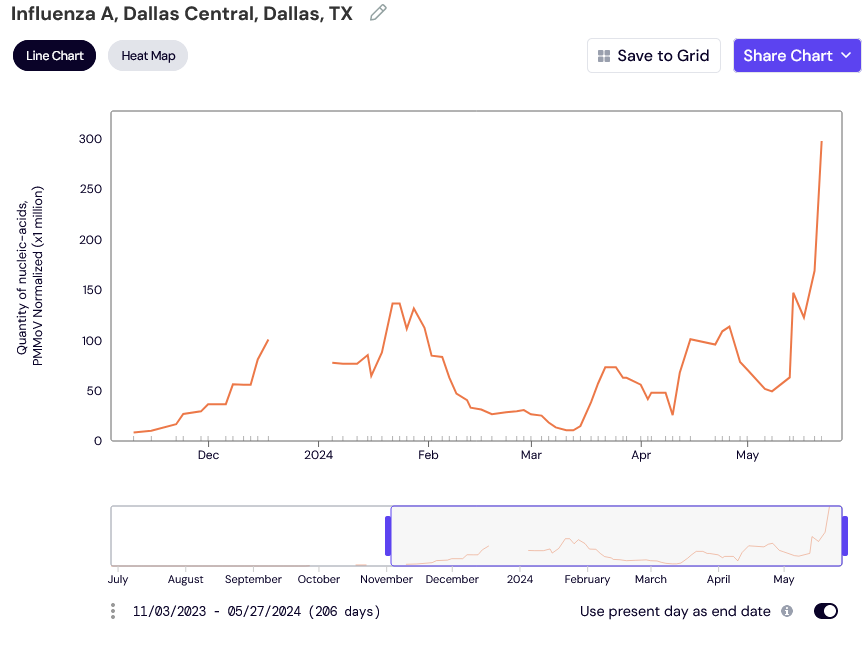
Before we get into the Michigan H5N1 case, it's important to highlight a significant spike in influenza A detected in the Dallas Central wastewater treatment plant in Dallas, TX. Although we do not yet know if this spike is due to H5N1, the localized surge surpasses the influenza A levels observed in the past 200 days, suggesting a potential H5N1 cause.
Currently, no known dairy farms are discharging into the Dallas Central wastewater treatment plant, so this spike warrants close monitoring. The CDC and USDA must investigate this unusual increase, though, as of today, no official information has been released from these agencies regarding their involvement.
The situation underscores the importance of proactive surveillance and rapid response to potential outbreaks. We must remain vigilant and ensure that thorough investigations are conducted to understand the source and implications of this spike in influenza A levels in Dallas.
Second Human Infection
A Michigan farm worker has tested positive for bird flu, making it the second human case in the U.S. during the current outbreak. The individual, who had contact with infected cows, experienced mild symptoms of an eye infection and has since recovered. While a nasal swab was negative, an eye swab confirmed the presence of the virus, highlighting the need to swab the eyes for testing and monitoring. This is an extremely important point that must be shared and adopted as the testing method for H5N1.
Michigan’s Response
Michigan's Department of Agriculture and Rural Development (MDARD) is actively implementing a proactive, science-based strategy to control the spread of influenza A (H5N1). This strategy incorporates a "one-health" approach, collaborating with federal, state, and local partners to address both animal and public health concerns swiftly.
To bolster these efforts, three U.S. Department of Agriculture (USDA) emergency management teams are on-site, providing daily support at affected poultry facilities across the state. Additionally, a USDA epidemiological team is working to trace and test within dairy herds, offering real-time data to manage the situation effectively.
Michigan’s Director Boring has taken action by signing a "Determination of Extraordinary Emergency" order on Wednesday, May 1st. This order strengthens Michigan's measures to protect the state's poultry and livestock industries from the ongoing threat of H5N1 and complements the USDA's federal order issued on April 24th.
MDARD has confirmed cases of influenza A (H5N1) in both dairy and poultry farms across several Michigan counties. However, the risk is not confined to these areas, and so far, we haven’t seen any testing beef cattle.
source: https://www.michigan.gov/mdhhs/inside-mdhhs/newsroom/2024/05/22/influenza-a-detection
Retail Dairy Product Testing
Between April 18-22, 2024, the FDA collected 297 samples of dairy products from retail locations across 17 states. Encouragingly, these tests did not detect any live, infectious virus. However, further studies are necessary to understand the potential impact of inactivated viral particles in dairy products. This includes investigating whether viral particles could survive the pasteurization process and their effects on the human digestive and immune systems.
We need to have a larger sample pool of whole milk from different time points. We need to know what, if any, impact large quantities of inactivated viral particles have on our digestive system and immune system.
We need to see the results from the muscle biopsies from the culled dairy cows that are likely entering the food supply as beef products. We need to randomly test calves, non-lactating dairy cows, and beef cows to quarantine them and all the cows they are with. We need to contain this outbreak before more people are exposed. The more people exposed the greater the odds of the virus evolving and gaining the capability for human-to-human transmission.
Source: "Characterization of highly pathogenic avian influenza virus in retail dairy products in the US" (5/21/2024) https://www.medrxiv.org/content/10.1101/2024.05.21.24307706v1 2.
On May 24th the National Institutes of Health released a report showing that high H5N1 influenza levels were found in mice given raw milk from infected dairy cows. “Mice administered raw milk samples from dairy cows infected with H5N1 influenza experienced high virus levels in their respiratory organs and lower virus levels in other vital organs.”
This is a very important message to share with anyone drinking raw milk. It is extremely dangerous and could help facilitate viral evolution that leads to human-to-human transmission. Drinking raw milk is not only extremely dangerous but it is an extremely selfish act that could jeopardize the lives of millions of people if the virus were to mutate within them.
Wastewater Surveillance Expansion
To track and control the spread of H5N1, WastewaterSCAN, a surveillance network led by Stanford University and Emory University in partnership with Verily Life Sciences, is scaling up its H5-specific testing. The network will analyze samples from 190 sewage treatment plants across 36 states, serving more than 42 million people. This will provide critical data, informing everyone of where outbreaks are occurring.
This was reported by Stat News.
Airborne transmission of H5N1
Recent research has highlighted the heightened pandemic potential of the H5N1 virus. Studies have shown that an isolate derived from mink can transmit through direct contact and airborne routes to ferrets, indicating the virus's adaptability and virulence. This underscores the need for ongoing efforts to control outbreaks and monitor viral evolution closely. "Risk assessment of a highly pathogenic H5N1 influenza virus from mink" was published on May 15, 2024.
"We show an H5N1 isolate derived from mink transmits by direct contact to 75% of exposed ferrets and, in airborne transmission studies, the virus transmits to 37.5% of contacts. Sequence analyses show no mutations were associated with transmission. The H5N1 virus also has a low infectious dose and remains virulent at low doses. This isolate carries the adaptive mutation, PB2 T271A, and reversing this mutation reduces mortality and airborne transmission. This is the first report of a H5N1 clade 2.3.4.4b virus exhibiting direct contact and airborne transmissibility in ferrets. These data indicate heightened pandemic potential of the panzootic H5N1 viruses and emphasize the need for continued efforts to control outbreaks and monitor viral evolution."
TACT’s Overview
The confirmation of a second human H5N1 infection in Michigan and the detection of the virus in dairy products underscore the persistent threat of bird flu. While current data offers some reassurance, it is clear that more research and vigilant surveillance are necessary. By expanding wastewater testing and closely tracking the virus's evolution, we can gain a better understanding of the risks posed by H5N1. However, this alone is not sufficient.
We need to implement random testing for farm workers, particularly those showing symptoms, to assess potential asymptomatic spread and ensure prompt isolation and containment should the virus mutate to enable human-to-human transmission.
Additionally, all beef and dairy cattle must be tested before crossing state lines and subjected to random testing within each state. Workers in slaughterhouses should also undergo regular testing to mitigate risks.
While there isn’t any evidence of human-to-human transmission at this time, the direction of evolution strongly suggests that this will occur unless government agencies, corporate farms, and smaller family farms all work together to contain the current outbreak among cows. Raising public awareness and taking proactive measures, such as ensuring farm workers wear appropriate personal protective equipment (PPE), are essential steps in protecting health and preventing another potential pandemic.
By subscribing, you’re helping support:
Unbiased reporting: We cut through the noise and deliver critical information you need to make informed decisions about your health.
In-depth analysis: TACT goes beyond headlines to uncover details and the true impact of COVID, Bird Flu, Monkeypox, and other emerging or evolving diseases.
Empowering insights: We translate complex scientific data into actionable knowledge, putting you in control of your well-being.
Support Independent Journalism - Become a Paid Subscriber Today!





TACT...Here is a point that I think is concerning. The Michigan human case has a different mammalian adaptation gene (PB2 M631L) than the Texas human case (PB2 E627K). This is a little like chambering another round in our game of Russian Roulette.
This can't be good...Coinfection of H5N1 w/SARS-CoV-2...
https://www.hindawi.com/journals/tbed/2024/8819622/