Despite Mild Symptoms, COVID can cause Erectile Dysfunction (E.D.), Lower Testosterone Levels and Reduced Sperm Count
Erectile dysfunction may be caused by vascular damage, but there are treatments available to help it heal.
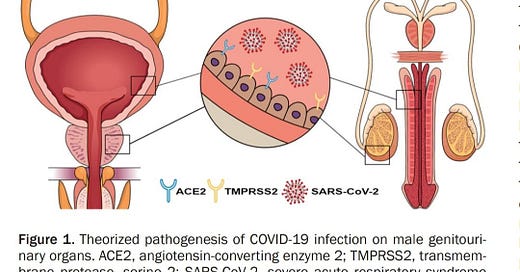
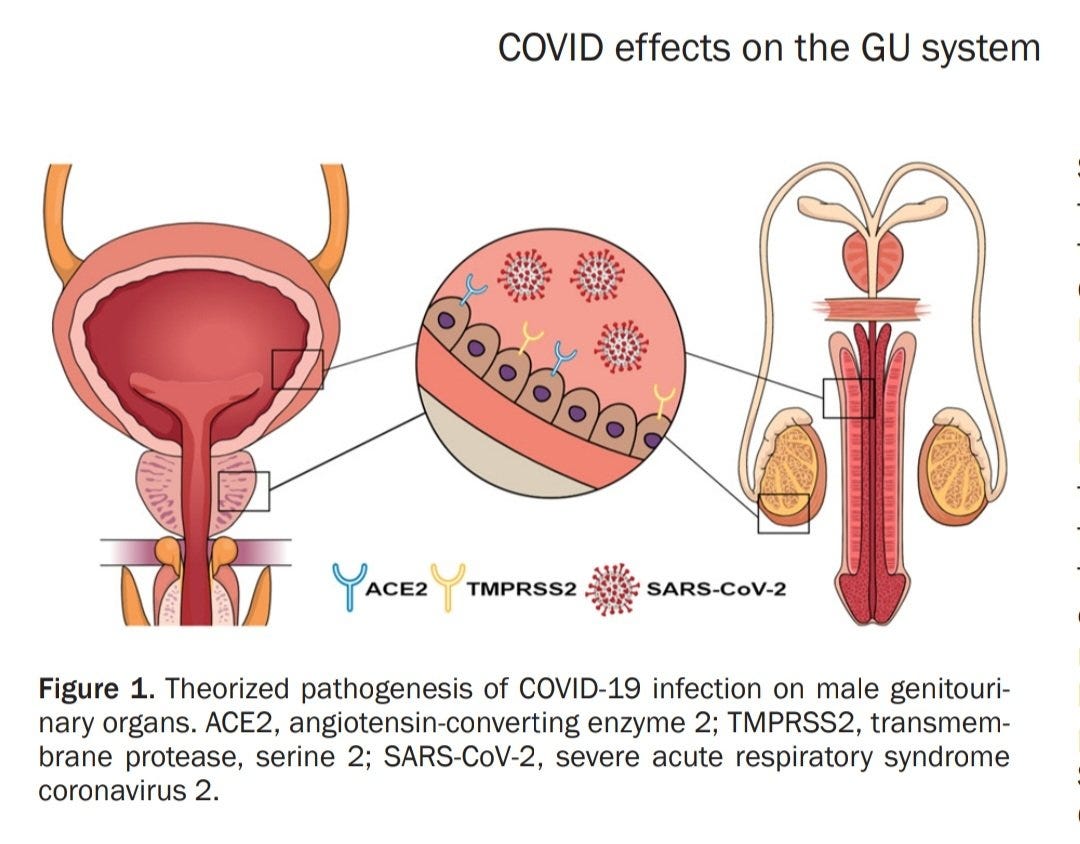
A study published August, 2022 reviews the evidence on how COVID affects the male genitourinary system. Genitourinary refers to the urinary and genital organs. "Evidence has revealed how COVID can affect the male genitourinary system & given the expression of TMPRSS2, this makes for a perfect viral reservoir." Since the tissue provides the necessary proteins for viral entry, the virus is detectible in the urine, but supposedly not in semen. The number of patients experiencing lower urinary tract symptoms (LUTS) is increased. “In addition to urinary symptoms, sexual symptoms have also been reported with decreased sperm numbers and erectile dysfunction. Overall, there is a significant burden that SARS-CoV-2 is placing on the genitourinary system."
Let's look at some of the earlier studies from various sources to get a sense of the overall picture. Prior to vaccines, a study titled "Impaired spermatogenesis in COVID-19 patients" found that 39% of men had lower sperm counts in their ejaculate. In 60.9% of the men, there was a significant increase in leucocytes in the sperm. Leucocytes are involved in the defense against foreign substances and viruses. It appears that they are present to combat the infection in the testicles. It was also noted that some of the men had autoimmune orchitis, or testicular inflammation.
A systematic review of how COVID affects the male reproductive system was published in May 2021. It states, "Fever and inflammation may be associated with poor sperm quality. Pathological examination of the testis/epididymis revealed that SARS-CoV-2 viral particles were present in 10 testicular samples, and the testis' spermatogenic function was impaired." They concluded that "the likelihood of SARS-CoV-2 in the semen of COVID-19 patients is very small, and semen should rarely be regarded as a carrier of SARS-CoV-2 genetic material. COVID-19, on the other hand, may cause testicular spermatogenic dysfunction through immune or inflammatory responses."
Spermatogenic Dysfunction
What is spermatogenic dysfunction? Sperm disorders include defects in the quality or quantity of sperm produced and defects in sperm emission. Diagnosis is by semen analysis and genetic testing.
This study published in March 2021 provides a little more insight into spermatogenic dysfunction. “Infertility affects up to 15% of couples worldwide, with up to 50% of cases attributable to male factor infertility [1]. In a majority of cases, the precise etiology underlying infertility in the male partner remains unclear. A subset of men with infertility has no sperm in the ejaculate, known as azoospermia, which may further be classified into obstructive (OA) or non-obstructive azoospermia (NOA). The majority of cases of NOA are idiopathic, however, some known etiologies include genetic disorders, chemotherapy or radiation, developmental or structural abnormalities, and hormonal imbalances. Despite the etiology underlying the spermatogenic dysfunction resulting in Non-obstructive azoospermia (NOA), or lack of sperm in the ejaculate due to spermatogenic dysfunction, sperm often can be surgically extracted from the testis for use in assisted reproductive technology (ART) with varying success.” That doesn’t sound great but at least there is still a chance of being a father if all else fails.
Now that we've covered the fundamentals of spermatogenic dysfunction, let's look at the worst-case scenario. This gives perspective, and hopefully, things will only get better from here. So, how did COVID affect the testicles of men that died from COVID? In July 2021, a study that described the testicular pathology of fatal COVID cases during autopsy’s found “viral particles in the cytoplasm of fibroblasts, endothelium, Sertoli and Leydig cells, spermatids, and epithelial cells of the rete testis” It concludes, "a combination of orchitis, vascular changes, basal membrane thickening, & reduced spermatogenesis associated w/COVID infection that may impair hormonal function and fertility in men." In other words, this is saying that men may have inflammation in one or both testicles, reduced blood flow (E.D.), reduced testosterone, and a reduced sperm count. So, yea, that checks off all of the things we don’t want to hear might be a result of COVID infections.
In February 2022, this study found that the testes could be a viral reservoir for SARS-CoV-2 replication. They also produced similar results to previous studies. “The testes of COVID-19 patients showed fibrosis, vascular alteration, inflammation, tunica propria thickening, Sertoli cell barrier loss, germ cell apoptosis, and inhibition of Leydig cells. Further, the intratesticular testosterone levels in the testes of COVID-19 patients decreased 30 times.” Let's go over that last sentence again. They found testosterone levels in the testicles were 30 times less than normal. That is a huge decline. Even if it were half as bad, that is still bad.
These were some of the worst-case scenarios, but how likely are these things to happen in men with mild symptoms?
A study published in August 2022 that looked at sperm quality three months after symptoms resolved gives us some hope. After three months, the men's testicular function had returned to within normal ranges in the majority of cases. The more severe the case, the more likely it is that men will have low sperm counts. A significant issue to consider is that many people are becoming infected every 3 or 4 months, and the rate is increasing now that COVID variants are evading antibodies from recent infections. We still don't know what the consequences of repeated infections will be. These studies were completed when the variants weren’t as evolved to evade antibodies and attack the immune system cells so it leaves a lot of questions regarding a very important function to our long-term survival.
The bad news from this study is that up to 30% of men experienced erectile dysfunction following COVID. We'll look at a specific case of erectile dysfunction below, which will provide more insight into what is happening to many men.
Persistent Infection
If COVID is making a home in testicles, using it as a hideout from the immune system, and replicating in a safe space, it wouldn’t be the first virus to do this. Some other viruses that have viability in the testes are Zika, HIV and the Ebola virus. Ebola has been isolated in semen as long as 82 days after symptoms onset. We know that HIV and Zika can be sexually transmitted but as of this writing, there hasn’t been any conclusive evidence showing sexual transmission of COVID. “Testicles protect viruses from immune attack, foiling attempts to destroy the pathogens.” COVID could use the testicles in the same way, persisting and replicating long after initial symptoms started and stopped.
In March 2022, a study looked at how COVID impacted male reproduction function. It warns us that"even though the patients of COVID appear to have recovered clinically, biological processes such as reproduction may be compromised." The study shows a "significant alteration of reproductive function at the molecular level and identifies several dysregulated proteins" It concludes, "These findings indicate the systemic dysfunction of the reproductive system in COVID-19-recovered males."
Erectile Dysfunction
A study published January 24, 2023, looks at persistent erectile dysfunction after COVID in a 35-year-old, non-smoker. He had been married since 2015 and never suffered from ED prior to COVID. He had mild symptoms, only suffering a cough and fever. Three weeks after his symptoms resolved he couldn’t get an erection. He tried many times over several weeks but wasn’t having any luck so he decided to seek help.
The doctors performed some tests. He lacked Vitamin D and had a low testosterone level. This is what we might expect after reading the preceding information. Over the next two months, they increased his vitamin D and testosterone levels. He did not, however, improve. Throughout this ordeal, he was most likely experiencing inner turmoil, self-doubt, and terrible insecurity. This type of situation could have disastrous mental health consequences for a younger man who does not have health insurance and does not go to the doctor. They may be afraid to say anything and prefer to keep it to themselves.
Doctors recommended that the 35-year-old undergo a penile ultrasound. Many men may find the idea of getting an ultrasound very intimidating. Though maybe he didn't hesitate, perhaps he struggled and found the courage to go, but it was a good thing he did because it confirmed endothelial damage in the penile vascular tissue. That would be a disturbing diagnosis for anyone, but fortunately for this man, his doctors had a plan.
A treatment for Erectile Dysfunction caused by endothelial damage in the penile vascular tissue.
They decided to offer low-intensity shockwave treatment after he rejected other ideas from his doctors (LI-SWT). He agreed to it and underwent six consecutive weekly LI-SWT sessions of 20 minutes each, totaling 4000 pulses. with an energy density of 0.09 mJ/mm2 and a frequency of 8 Hz. They used linear-focused piezo shockwaves (Linear Shockwave Tissue Coverage-Erectile Dysfunction, LSTC-ED, Richard Wolf GmbH, Knittlingen, Germany). Therapy with tadalafil daily 5 mg was started for four months according to the previously published procedure.
He reported "no adverse events and a good improvement in the frequency and quality of his erections" at the 6-month follow-up. He returned after 12 and 18 months and reported that everything was functioning normally. After 18 months, the doctors requested that he have another penile duplex ultrasound. It demonstrated a restoration of penile vascular function.
If the doctors say it's just hormones and/or vitamins and increasing them doesn't help, request an ultrasound to see if there is endothelial damage in the penile vascular tissue. Fortunately, the treatment plan worked for this individual. Hopefully, this can help someone who believes it's all in their head or is feeling bad about themselves.
Men of all ages should be aware of this potential situation following COVID. It could help limit the mental distress they may end up causing themselves. If the figures are correct and 20% to 30% of men will be dealing with this after COVID, then there will be a lot of men likely keeping it to themselves. We don't have data on how this might affect young men in their late teens or early twenties but we shouldn't assume it can't happen. We should assume it will. They would be more likely to struggle with the insecurities that come with confronting something like this on their own while not understanding what is causing it. This is something to keep in mind as COVID spreads at an unprecedented rate. As time passes, this will undoubtedly affect an increasing number of men.
There are still a lot of unanswered questions. We have no idea how this may impact younger boys’ future chances at reproduction. How much does the risk increase if repeatedly infected? If a sixteen-year-old is infected 20 or 30 times before they want to have children in their late 20s or early 30s, then what are the odds they will be able to have viable sperm? Will it be necessary to freeze sperm when a teen, just to have any hope of having children later in life? These are realistic questions we have to start thinking about and finding the answers to if this continues as it likely will for the foreseeable future.
The government, public health, and the major media outlets would like us to believe that COVID has become less dangerous and is not a significant concern. The media reports have dwindled and when they do report anything, it is often delayed and misleading. It is more important than ever to have independent sources that are not beholden to large donors, political parties, or any other group to remain focused on providing the latest science and data so that we may achieve a sustainable path forward. Sign up as a paid subscriber today and/or consider giving a gift subscription. Thank you for your support.





"Men experience a long-term drop in semen quality after COVID infection – even if the infection was mild"
(26-JUN-2023)
https://www.eurekalert.org/news-releases/993399