COVID: Unveiling the Next Wave -The Rise of KP.2.3 and LB.1 Variants. How a New Mutation in KP.2.3 Could Impact B-cells
Wastewater Prevalence Beginning to Increase in The North East U.S.
The LB.1 and KP.2.3 variants have swiftly spread across the globe in just a few weeks and currently have the highest growth rates. There have already been 42 sequences of LB.1 and 50 of KP.2.3 from the U.S. Later, we'll list all the countries where these variants have been identified and go into more detail on the new mutation found in KP.2.3 and its implications.
Let's begin by examining the prevalence of wastewater indicators in the U.S. In the Northeastern United States, there's a modest increase noted, with certain areas experiencing faster rises than others. This trend is expected to persist as the KP.2 variants gain ground, especially since most schools are slated to remain open until June. Following the conclusion of the academic year, the Northeast may witness a decline, only to see numbers rise once more into later June as summer programs and camps are underway. Meanwhile, in the Southern United States, indications suggest that the summer surge may commence by late May into early June.
COVID prevalence will very likely increase quite a bit higher than last summer.
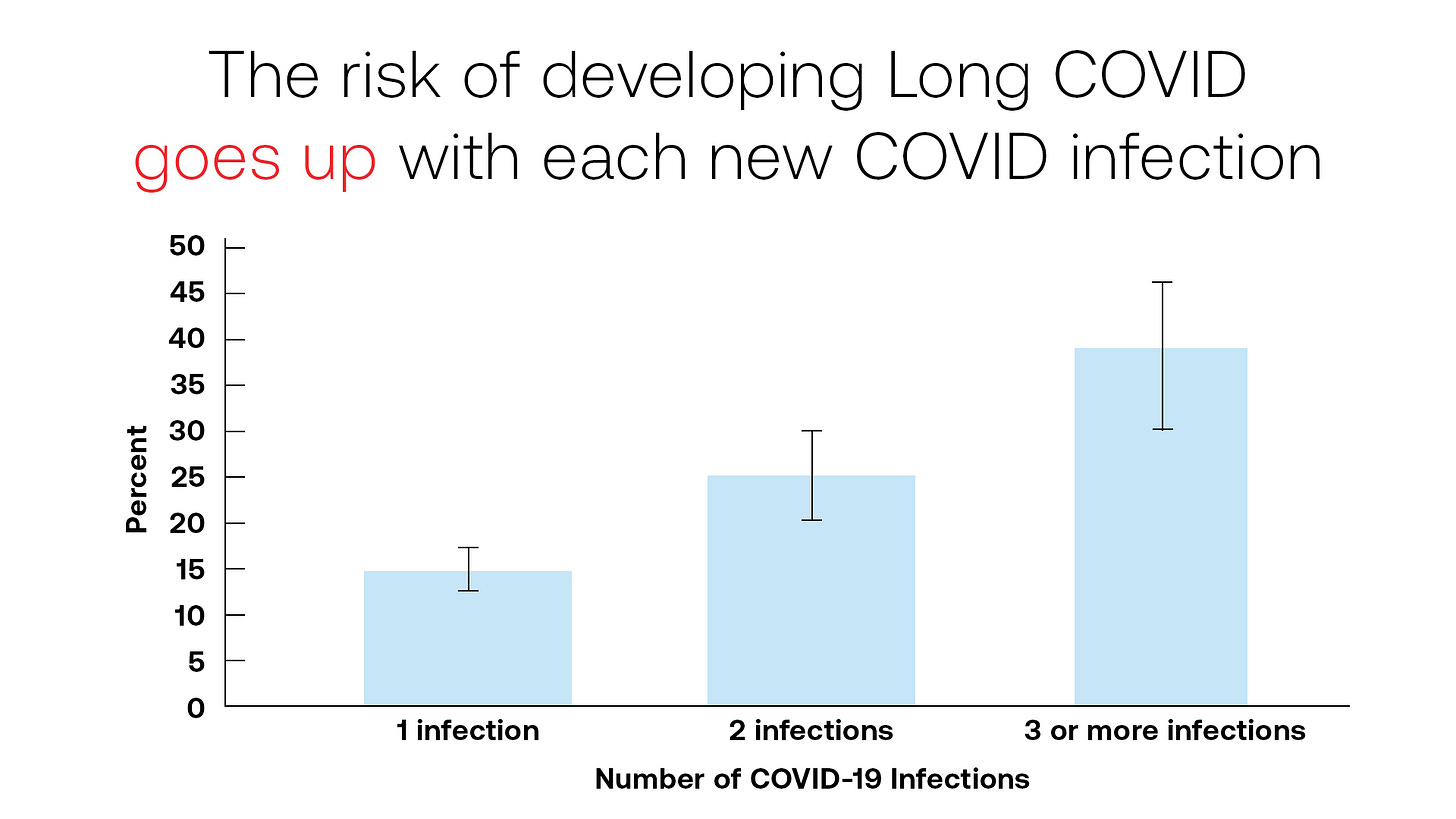
On Long COVID Awareness Day, Moderna highlighted a concerning trend: the likelihood of experiencing Long COVID symptoms rises with each new infection, as illustrated in the graphic below. They reference a Canadian study published on December 8, 2023, revealing that as of June 2023, 2.1 million individuals continued to suffer from Long COVID symptoms. Alarmingly, nearly half of these individuals reported no improvement in symptoms over time, underscoring the gravity of the situation. Sadly, the KP.2 variants are very likely to cause hundreds of thousands, if not millions, of new cases of persistent infections, exacerbating the burden of Long COVID.
To be clear, KP.2 and its offspring, KP.2.1, KP.2.2, and KP.2.3 are poised to bring about considerable avoidable illness this summer with acute infections. As we move into the fall, many individuals may come to grips with or not understand the connection to the fact that they are grappling with new-onset symptoms of Long COVID.
Below, the Yale School of Public Health points out that 5 - 20% of people develop lingering symptoms or new health problems, called Long COVID. As of March 2024, 30% of all American adults who have had COVID have experienced Long COVID.
Spread the word about TACT to a friend and contribute to keeping more people informed about the latest information.
The KP.2 variants are currently dominating the scene, and they're expected to remain prevalent for at least the next few months. However, there are other variants lurking in the shadows and entering the mix. These variants possess a higher growth advantage and carry mutations within the virus's structure, potentially leading to more severe illness in some individuals.
As summer progresses, we anticipate the increasing prevalence of variants like KP.2.3 and LB.1. These variants, particularly LB.1 and KP.2.3, currently exhibit the highest growth advantages. Despite being relatively new, they have already spread to numerous countries worldwide, indicating their ability to rapidly spread. This is occurring amid a notable decrease in genomic sequencing, suggesting that their spread may extend beyond what is currently observable.
Of particular concern is KP.2.3, which harbors a novel mutation in ORF3. This mutation might enable the virus to evade recognition by B-cells, hindering the immune response. We will highlight an insightful study that shows the ORF3 mutation in an extinct variant from earlier in the pandemic. The same study shows that the variant was effectively eliminated through non-pharmaceutical interventions. Unfortunately, we aren’t going to stop it this time.
By subscribing, you’re helping support:
Unbiased reporting: We cut through the noise and deliver critical information you need to make informed decisions about your health.
In-depth analysis: TACT goes beyond headlines to uncover details and the true impact of COVID, Bird Flu, Monkeypox, and other emerging or evolving diseases.
Empowering insights: We translate complex scientific data into actionable knowledge, putting you in control of your well-being.
Support Independent Journalism - Become a Paid Subscriber Today!
KP.2.3 (JN.1.11.1.2.3)
KP.2.3 with a defining mutation at ORF3a:K67N
A case study on an outbreak in Colorado Springs published on October 4, 2022 says, “The ORF3A/K67N mutation results in a change from a positively charged residue to an uncharged, polar residue. This particular residue occurs in an LKK peptide motif that is predicted to be a likely B-cell epitope by Azad and Khan, 2021. Because the mutation seems to increase the free energy of folding, it has the potential to alter a putative B-cell epitope, allowing the virus to better evade host immune responses.”
Here’s a more simplified explanation of what that means. B-cells are a type of immune cell that produce antibodies, which are proteins that help the body fight off infections. When a virus enters the body, B-cells can recognize specific parts of the virus called epitopes. These epitopes are like a "flag" that tells the immune system to attack the virus.
In the case of the ORF3A/K67N mutation, it occurs in a part of the virus that is predicted to be a B-cell epitope. This means that the mutation changes the shape or structure of this epitope. If the mutation increases the free energy of folding, it might alter the shape of the epitope in a way that makes it harder for B-cells to recognize it. As a result, the virus could potentially evade detection by the immune system's B-cells more effectively, making it more challenging for the body to mount an effective immune response against the virus.
This is the only study that came up in the search and as we see below they successfully utilized infection control strategies to stop the spread of this variant.
The study says that they were able to link multiple infections back to a rapid spreading event in late October 2021, which resulted in the strain clusters A12 and A13. “Following the dramatic increase in infections, further lockdown measures were implemented at USAFA limiting new community introductions. At the end of the semester, a similarly rigorous testing and quarantine process occurred prior to release for the winter break, likely eliminating the strain from circulation within the population.” They went on to say that “luckily, it appears to have been contained by the rigorous epidemiological control procedures (e.g. social distancing, mask wear, limited gathering, virtual learning) employed at the USAFA.” It doesn’t look like we will be able to contain it this time around.
KP.2.3 has been sequenced in Australia, Canada, Denmark, France, Germany, India, Japan, Netherlands, New Zealand, Singapore, Sweden, the U.K., and 50 cases in the U.S. already. When we consider the limited sequencing occurring, we can assume it has spread further and the numbers are much higher.
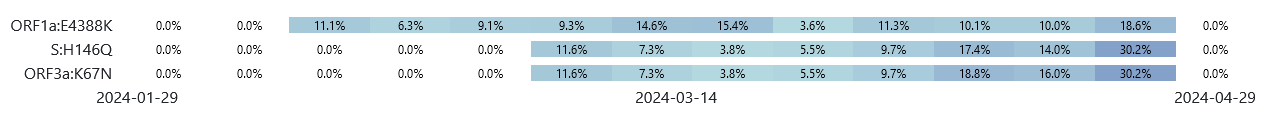
The graphic below shows that the ORF3a: K67N mutation, along with S: H146Q and ORF1a: E4388K mutations have been steadily increasing in the number of sequences of KP.2.
In KP.2.3 the ORF3a: K67N mutation and the S: H146Q mutation are in 100% of those sequenced. Interestingly, the ORF1a: E4388K, is only showing up in 6% of the KP.2.3 sequences. The graphic above helps show that KP.2.3 began its journey in late March and has been steadily gaining a larger portion of the KP.2 sequencing. This shows that these mutations give KP.2.3 a clear advantage. Unfortunately, it appears that the advantage involves being better adapted to evade and suppress the human immune response, increasing the likelihood of persistent infections.
LB.1 (JN.1.9.2.1)
Let’s review where it has already been sequenced. Australia- 4 cases, Canada - 9 cases, France - 2 cases, India -1 case, Ireland - 1, Japan - 2, Pakistan - 1, Sweden - 2, Taiwan -1, United Kingdom - 9, and the United States with 42 cases.
Comparing KP.2 to LB.1
Both have S:R346T & S:F456L (FLIRT)
The number of mutations for each variant:
LB.1 has 81 mutations.
KP.2 has 97 mutations.
Mutations unique to LB.1:
LB.1 mutations not present in KP.2:
ORF1a:L1507F (21%), ORF1a:P2287H (8%), ORF1a:S2517P (8%), ORF1b:T1555I (26%), ORF1b:G2068R (4%), S:I670M (8%), S:Q183H(100%)
% = percentage of sequences that have that mutation
The number of Spike gene mutations for each variant:
LB.1 has 54 mutations in the S gene.
KP.2 has 57 mutations in the S gene.
S gene mutations notes:
LB.1 doesn’t have S:K187R, S:V1104L
LB.1 acquired S:I670M (8.7%) , and S:Q183H (100%)
S:Q183H note: S:Q183E was found in XBB.1.5: A change from S:Q183E to Q183H indicates a substitution of the amino acid glutamine (Q) at position 183 in the spike protein (S) with histidine (H). Implications are still unknown.
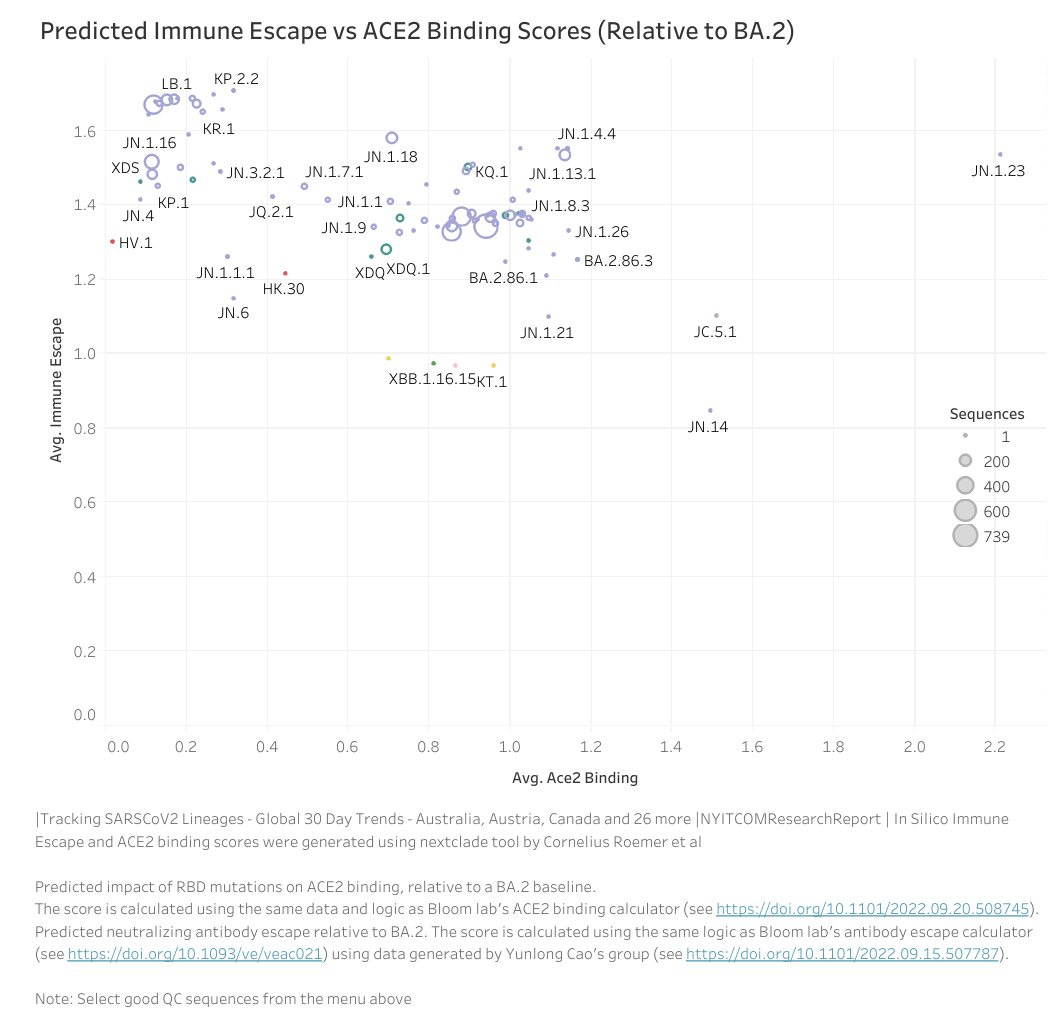
LB.1 Immune Escape
KP.2.2 and LB.1 rank highest in immune escape scores, indicating their enhanced capability to evade and infect the immune system, thereby increasing the likelihood of viral persistence. Although KP.2.3 has yet to receive a score, it's anticipated to surpass KP.2.2 in immune evasion potency.
It's still too early to determine whether KP.2.2 or KP.2.3 will surpass and overpower LB.1, but either way, these are all variants with a greater ability to evade and suppress the immune system, increasing the risk of persistent infections. Once the virus takes hold, it becomes challenging to eliminate and currently impossible for many people to effectively eliminate it from their bodies.
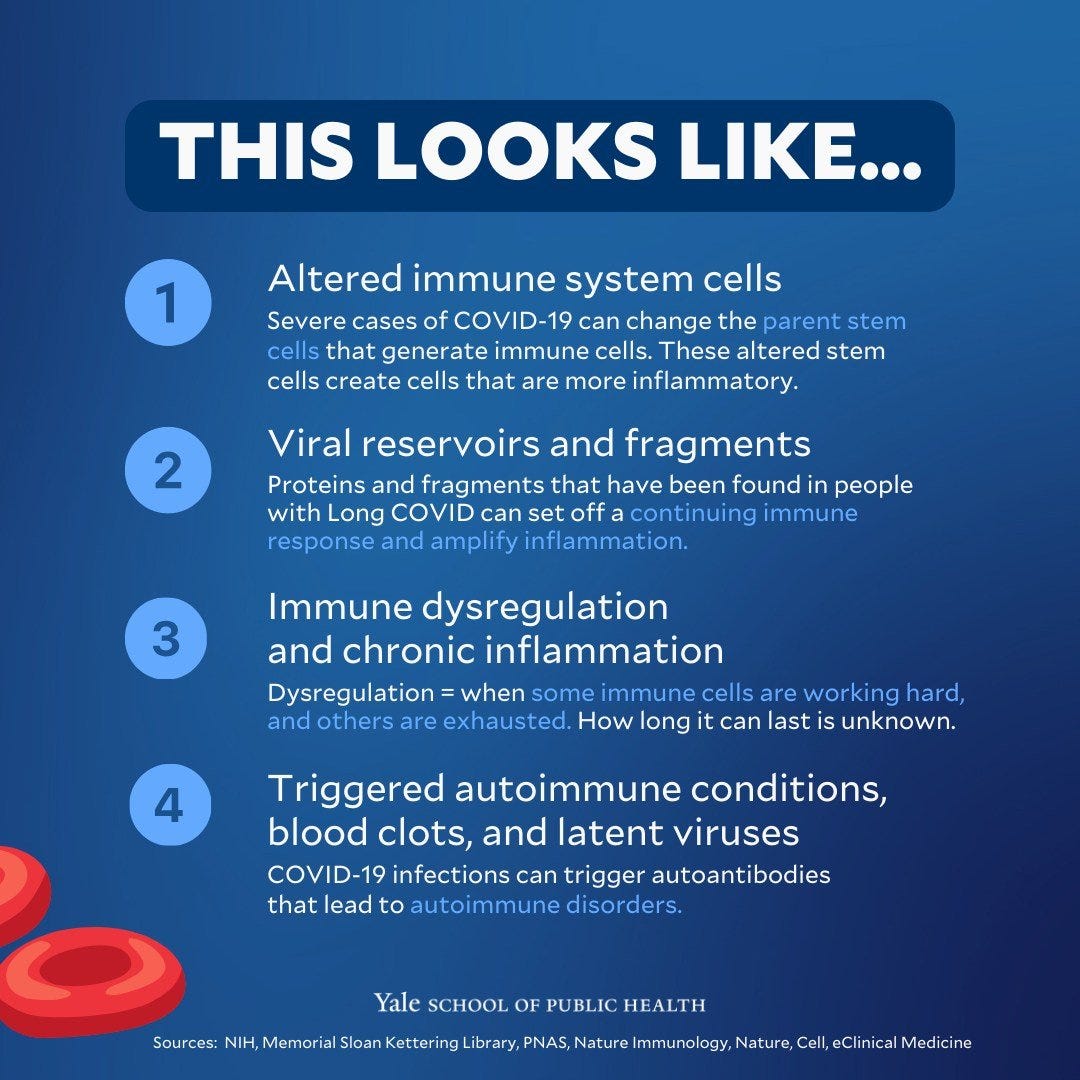
As depicted in the graphic from the Yale School of Public Health, COVID-19 infections inflict significant harm on the immune system. Persistent infections trigger an ongoing immune reaction, exacerbating inflammation and frequently culminating in autoimmune conditions.
Mitigating Risk
We can effectively reduce our risk of exposure by employing several measures, such as using high-quality N-95 masks, gargling with mouthwash containing CPC, using saline nasal spray and rinse, and promptly showering upon returning home. When outdoors, it's advisable to briefly hold your breath when passing others and be mindful of wind directions. Despite diligently following these precautions, some individuals may still become infected. However, by minimizing the viral load we encounter, we enhance our body's ability to mount a robust immune response because it isn’t being overwhelmed. Let's stay vigilant and prioritize safety. We must work together against COVID transmission.








Please keep reporting. Your summaries are the only information that I get on public health concerns.
Did you see the news that cancer rates will be at all time high this year? But no one knows why. 🤦🏾♀️
Sarscov2 changes our dna. Sarscov2 stays in our bodies and causes non-stop inflammation- mcp1 is in hyperdrive and causes cancer.
There are 3 that are close friends or close relatives who have been diagnosed with stage 4 cancer since 2021. Lung, esophageal, ovarian. My dear friend thought her lung cancer was allergies- she never smoked or vaped. My brother in law’s twin asked the doctor about the lump in his throat in Dec 23. Doctor said it couldn’t be cancer. Poor man is finally starting treatment this week. Chemo, radiation and then hopefully surgery- but he will lose his vocal cords. He is 49.
We know why cancer rates are increasing- we don’t want to talk about it. Covid causes cancer.