COVID Induced Fetal Brain Hemorrhage
Placental lesions occur despite mild maternal COVID-19 symptoms.
Several viruses have been shown to cross the placenta. When the infection happens early in the pregnancy, it is more likely to hurt the brain. Congenital infections occur in utero. Some of the more prevalent ones are known by the acronym TORCH (Toxoplasma gondii, rubella virus, cytomegalovirus (CMV), and herpes virus), as well as Zika virus infection. (1) COVID can now be added to this group as well. The question that needs to answered is how frequently is this occurring? It seems likely that COVID will have much better odds than any of the others at infecting all but the most careful pregnant women.
Other viral infections occur within days to weeks after the birth of the infant and are referred to as perinatal infections. Some of these perinatally acquired infections (parechovirus, enterovirus (EV), rotavirus, and others) may result in injury to especially the white matter in the brain.(1)
A study published in Brain, January 16, 2023, says, “We report the presence of SARS-CoV-2 in first- and second trimester fetal brain tissue in association with cortical hemorrhages.” (2)
This research team studied 661 human fetal tissue samples taken between July 2020 and April 2022. In 21 months, COVID was found in the brains of all 26 babies that died of a brain hemorrhage, before birth. In comparison, “only two cases of similar hemorrhages in cortical tissue were observed from images of 300 randomly selected samples from a total of 4917 that were collected between September 1999 to December 2019.”(2) A larger sample size over a 10 year period only found 2, while a much smaller sample size over 21 months found 26 that were all positive for COVID in their brains.
The samples were received during periods when confirmed COVID cases were at their highest. This could show that exposure to higher viral loads plays a role otherwise why would they occur from peak periods. We will need more data to know that answer. The fact that COVID is infiltrating their brains is very concerning.
“Our results suggest that there is an association between early development of human fetal brain tissue and susceptibility to COVID-19 infection,” says neurobiologist Marco Massimo from King’s College London."
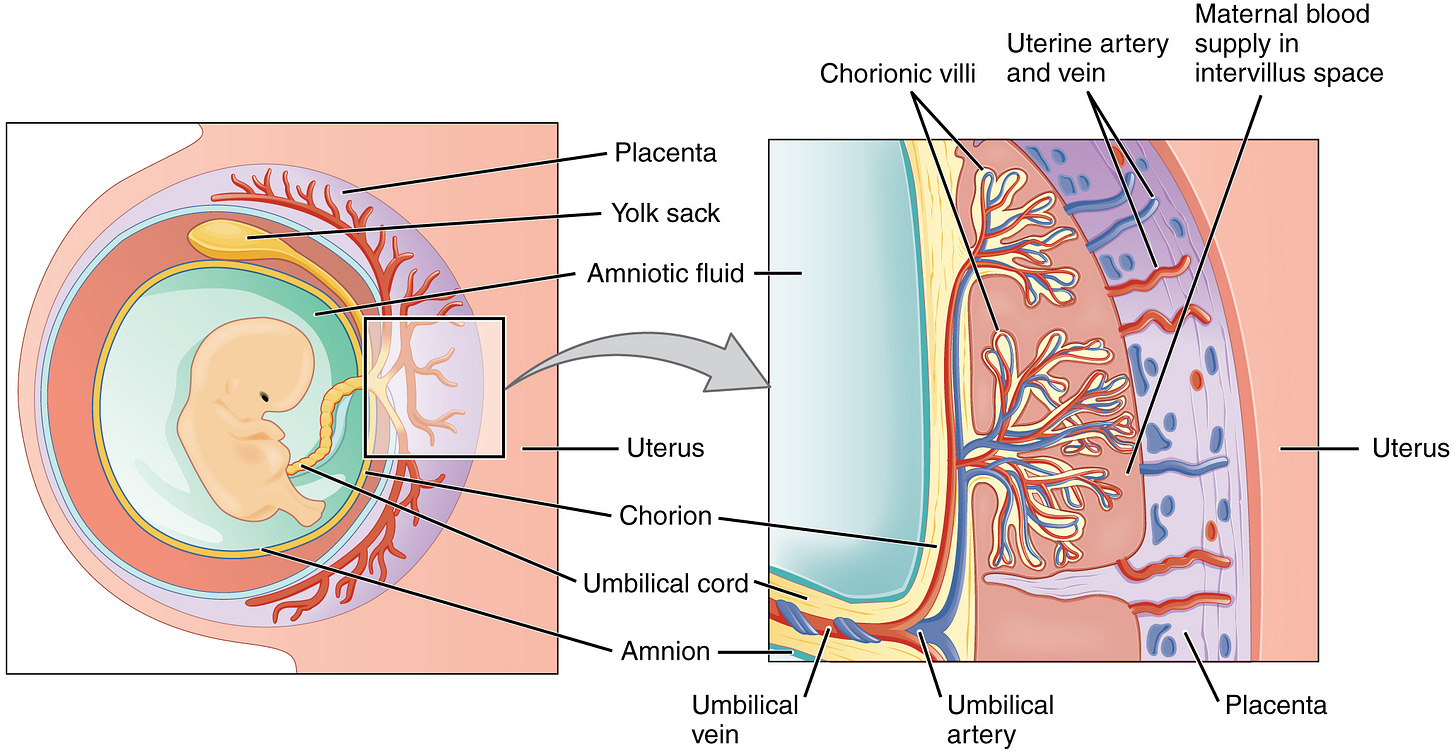
They found small amounts of COVID in tissue samples taken from the placenta, amnion, and umbilical cord. This isn’t the first study to find COVID in the placenta. In a study published in March 2022, they said, “We were able to detect the virus (COVID) in the oesophagus, large intestine, kidney, placenta, lung, and brain." (3)
Here is one more study the shows COVID infects throughout the body, and brain for months. "SARS-CoV-2 infection and persistence throughout the human body and brain" “We detected SARS-CoV-2 RNA in multiple anatomic sites, including regions throughout the brain, for up to 230 days following symptom onset. Our data prove that SARS-CoV-2 causes systemic infection and can persist in the body for months.” (4)
This is what they found with the less immune evasive variants. COVID has been found in adult brains and fetuses’ brains. It isn’t too hard to imagine that it is impacting children’s brains to varying degrees, but that hasn’t been proven yet.
Let’s take a look at some studies that have looked at how COVID is impacting pregnancy.
A study published in the European Journal of Obstetrics and Gynecology and Reproductive Biology, Volume 257, February 2021, found that only 25% of pregnant women with SARS-COV-2 infections who were admitted to the hospital to give birth showed symptoms. 75% of the pregnant women had no symptoms, so that means all pregnancies should be carefully checked to see if COVID poses any other health risks.
Importantly, they found that pregnant women who had COVID had a higher risk of bleeding after giving birth, needing a blood transfusion, and being admitted to the ICU than women who did not have COVID.
On July 28, 2021, A case study titled, “Severe fetal brain damage subsequent to acute maternal hypoxemic deterioration in COVID-19”, reviews what happened to a 36-year-old woman, who developed COVID-19 symptoms at 25 1/2 weeks of gestation. One week after admission, her oxygen saturation (SpO2) dropped suddenly to 87%, while she was receiving 3 L/min of supplemental oxygen. She was then moved to the ICU, where her lung function quickly got worse and she had to be intubated. She was able to pull out of it and get the tube removed (extubated). At 27 weeks, her baby was looking like everything was going to be okay.
Keep reading with a 7-day free trial
Subscribe to T.A.C.T. to keep reading this post and get 7 days of free access to the full post archives.